Whole community planning is an important
aspect of planning in emergency management. Individuals with functional and
access needs (IFAN) have become more engaged in the emergency planning process
as a result of lessons learned from Hurricane Katrina and other events.
Functional Needs Support Services (FNSS) is a component of emergency response
that can overwhelm local resources if there is not a plan in place to meet the
needs of the population.
According to the 2010 US Census: American
Community Survey, approximately 1.2 million (12%) Georgians are classified as
having some type of functional and/ or access need (hearing, visual, cognitive,
ambulatory, self-care, independent living). Nationally, it is estimated that
20% of the US population has some type of functional and/or access need. These
numbers are an indication of why it is important to consider the needs of the
whole community while planning for emergencies and disasters.
Planning for individuals with functional
and access needs (IFAN), with an emphasis on the provision of supportive
services in emergency shelters, has been at the heart of discussions within the
State of Georgia. State emergency planning partners within Georgia have been
working to address these concerns since 2006 when they came together to form
the State Americans with Disabilities Act (ADA) Working Group. At that time,
key emergency management stakeholders as well as disability service providers
began developing tools for local planners to aid with inclusive emergency
coordination during disaster incidents.
In 2010, the Working Group became the
Emergency Preparedness Coalition for Individuals with Disabilities and Older
Adults. The Coalition developed The State of Georgia Functional and Access
Needs Support Services Toolkit, hereafter called the FNSS Toolkit, to provide
resources and information for FNSS planning, with a specific emphasis on FNSS
shelter planning.*
The intent of this document is to assist
local officials with tools that will enable them to provide reasonable
accommodations for all citizens during disaster incidents. Specific examples
are given for older adults and people with disabilities, but those with
functional and access needs are a diverse part of every community. Working to
address these issues at each level of government will help to improve overall efficiency,
maximize resources, ensure equal access for all Georgians and ultimately enhance
statewide emergency preparedness.
* This toolkit is adapted from the State of
Texas Toolkit. Special Thanks to the State of Texas Functional Needs Support
Services Integration Committee.
This publication was supported in part by
the Cooperative Agreement Number TP12-1201 from The Centers for Disease Control
and Prevention and/or Assistant Secretary for Preparedness and Response. Its
contents are solely the responsibility of the authors and do not necessarily represent
the official views of the Centers for Disease Control and Prevention and/or
Assistant Secretary for Preparedness and Response.
|
AAA
|
Area Agencies on Aging
|
|
ACS
|
American Community Survey
|
|
ADA
|
Americans with Disabilities Act
|
|
ARC
|
American Red Cross
|
|
ASL
|
American Sign Language
|
|
AT
|
Assistive Technology
|
|
CART
|
Computer Assisted Real Time Translations
|
|
CDC
|
Centers for Disease Control
|
|
CERT
|
Community Emergency Response Teams
|
|
CIL
|
Center for Independent Living
|
|
CMS
|
Consumable Medical Supplies
|
|
COAD
|
Community Organizations Active in
Disasters
|
|
CPG
|
Comprehensive Preparedness Guide
|
|
DAS
|
(Georgia) Division of Aging Services
|
|
DBHDD
|
(Georgia) Department of Behavioral
Health and Developmental Disabilities
|
|
DFCS
|
(Georgia) Division of Families and
Children Services
|
|
DHS
|
(Georgia) Department of Human Services
|
|
DME
|
Durable Medical Equipment
|
|
DOJ
|
(U.S.) Department of Justice
|
|
EMA
|
Emergency Management Agency
|
|
ESF
|
Emergency Support Function
|
|
ESP
|
Enhanced Services Program Database
|
|
FEMA
|
Federal Emergency Management Agency
|
|
FNSS
|
Functional Needs Support Services
|
|
FODAC
|
Friends of Disabled Adults and Children
|
|
GaRRS
|
Georgia Radio Reading Service
|
|
GAO
|
Georgia Advocacy Office
|
|
GDPH
|
Georgia Department of Public Health
|
|
GDA
|
Georgia Department of Agriculture
|
|
GEMA
|
Georgia Emergency Management Agency
|
|
GIS
|
Geospatial Information Systems
|
|
GNAS
|
Georgia Nurse Alert System
|
|
ICS
|
Incident Command System
|
|
IMT
|
Incident Management Team
|
|
IFAN
|
Individuals with Functional and Access
Needs
|
|
JIC
|
Joint Information Center
|
|
LEOP
|
Local Emergency Operations Plan
|
|
LEPC
|
Local Emergency Planning Committees
|
|
LTRC
|
Long Term Recovery Centers
|
|
MOU
|
Memorandum of Understanding
|
|
NAMI
|
National Alliance on Mental Illness
|
|
OTC
|
Over-the-Counter Drugs
|
|
PAS
|
Personal Assistance Services
|
|
RLO
|
Regional Liaison Officer
|
|
RN
|
Registered Nurse
|
|
SOC
|
State Operations Center
|
|
SOP
|
Standard Operating Procedures
|
|
VOAD
|
Voluntary Organizations Active in
Disasters
|
The Emergency Preparedness Coalition for
Individuals with Disabilities and Older Adults (the Coalition) has played an
important role in the development of guidance to assist with planning
initiatives for individuals with functional and access needs.
The Coalition's purpose is to:
Serve as a comprehensive clearinghouse
between local advocacy groups serving individuals with disabilities and older
adults and Georgia agencies responsible for emergency preparedness under the
Georgia Emergency Operations Plan.
Promote and maintain an active dialogue by
serving as a conduit between individuals with disabilities and older adults,
and Georgia agencies responsible for emergency preparedness under the Georgia
Emergency Operations Plan.
Provide subject matter expertise to: (a)
Emergency response planners to ensure that all emergency plans incorporate the
needs of people with disabilities and older adults, and (b) Organizations
throughout Georgia that serve and advocate for people with disabilities and
older adults enabling them to share disaster preparedness and response
information with their constituencies.
Member Agencies:
Atlanta Area School
for the Deaf
American Red Cross
of Georgia
Center for Advanced
Communications Policy-Georgia Institute of Technology
Department of Human
Services, Division of Aging Services
Department of Human
Services, Office of Facilities and Support Services
DeKalb County
Emergency Management Agency
Federal Emergency
Management Agency
Friends of Disabled
Adults and Children
GACHI- Serving the
Deaf and Hard of Hearing
Georgia Advocacy
Office
Georgia Department
of Behavioral Health and Developmental Disabilities
Georgia Department
of Public Health, Division of Health Prevention, Emergency Preparedness and
Response
Georgia Emergency
Management Agency Georgia Radio Reading Service
Georgia State
Finance and Investment Commission-State ADA Coordinator's Office
Gwinnett County
Emergency Preparedness Coalition
Gwinnett, Newton,
Rockdale County Health Departments
Portlight
Strategies, Inc.
The Shepherd Center
Southeast
ADA Center
Tools
For Life-The Alternative Media Access Network, Georgia Institute of Technology Enterprise
Innovation Institute
Contact information for the
above agencies is in the appendices.
The Federal Emergency Management Agency's
(FEMA's) Guidance on Planning for Integration of Functional Needs Support
Services in General Population Shelters uses a functional needs framework to
determine which individuals might need help in an emergency. People who have
functional or access needs will need support services during a disaster. FNSS
are defined as services that enable individuals to maintain their independence
in a general population shelter. The purpose of this section is to provide
local jurisdictions with recommendations for meeting the needs of displaced
populations with functional and access needs in a disaster/emergency.
The support services include the following:
·
Reasonable
modification to policies, practices, and procedures
·
Durable
medical equipment
·
Consumable
medical supplies
·
Personal
assistance services
·
Other
goods and services as needed
The following individuals have worked to
adapt the Texas Functional Needs Support Services Toolkit to the needs and
resources in Georgia.
|
AGENCY
|
AGENCY REPRESENTATIVE
|
|
Department of Public Health- Division of
Health Protection, Emergency Preparedness and Response
|
Betsy Kagey, Co-Chair Academic and
Special Projects Liaison
|
|
Georgia Department of Human
Services-Division of Aging Services
|
Jennifer Hogan, Co-Chair Disaster Preparedness
Coordinator
|
|
Georgia Emergency Management Agency
|
Angela C. Barton Planning Section
Manager
|
|
Georgia Department of Human Services-
Office of Facilities & Support Services
|
Wendy Casey
Emergency Support Function 6 Coordinator
|
|
Georgia State Financing & Investment
Commission- State ADA Coordinator's Office
|
Mike Galifianakis State ADA Coordinator
|
|
Southeast ADA Center
|
Mary Morder Help Desk Specialist
|
|
GACHI-Serving the Deaf & Hard of
Hearing
|
Kevin Steffy
GATEDP Co-Coordinator, Outreach/
Training
|
|
Friends of Disabled Adults and Children
|
Ruth Rust
Disaster Assistance Coordinator
|
|
American Red Cross of Georgia
|
Marilyn Self
Manager-Disaster Readiness
|
The purpose of this toolkit is to provide
an overview of the information, products and services that are available within
the State of Georgia to assist local partners and disability community
stakeholders with Functional Needs Support Services (FNSS) planning. State
partners have worked together on various initiatives to address FNSS planning needs
locally, regionally and at the state level. This toolkit contains five
chapters:
1) Introduction
·
Overview
of the Emergency Preparedness Coalition for Individuals with Disabilities and
Older Adults Coalition
·
Overview
of Functional and Access Needs Support Services
·
Sheltering
Committee, Functional Needs Support Services Subcommittee
·
Purpose
and Scope of the Functional and Access Needs Toolkit
·
Legal
Authority
·
The
State of Georgia Functional and Access Needs Definition
2) Including
Individuals with Functional and Access Needs (IFAN) in Emergency Management
Planning
·
Step
1: Complete an Emergency Planning Assessment
·
Step
2: Identify Potential Mass Care Partners
·
Step
3: Review and Analyze IFAN Statistics for the Community
·
Step
4: Identify and Invite IFAN Partners to the Planning Table
·
Step
5: Identify FNSS Resources for Planning
·
Step
6: Special Considerations to Effectively Include IFAN in your Planning
3) Overview of
Sheltering in Georgia
·
Overview
of Sheltering in Georgia
·
Process
for Opening a Shelter
·
American
Red Cross Progression of Shelter Alert/Activation
·
Shelter
Staffing Recommendations
·
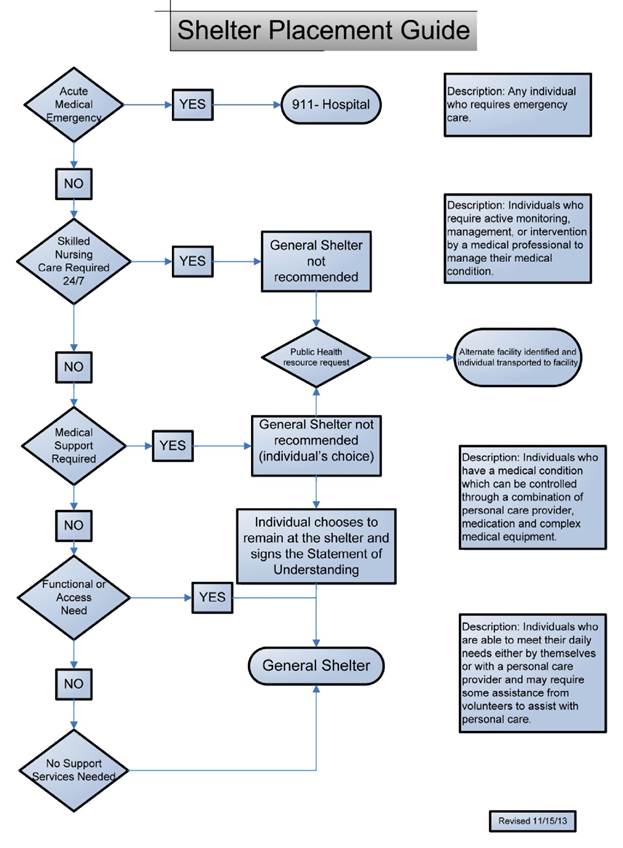
Shelter
Placement Guidance
·
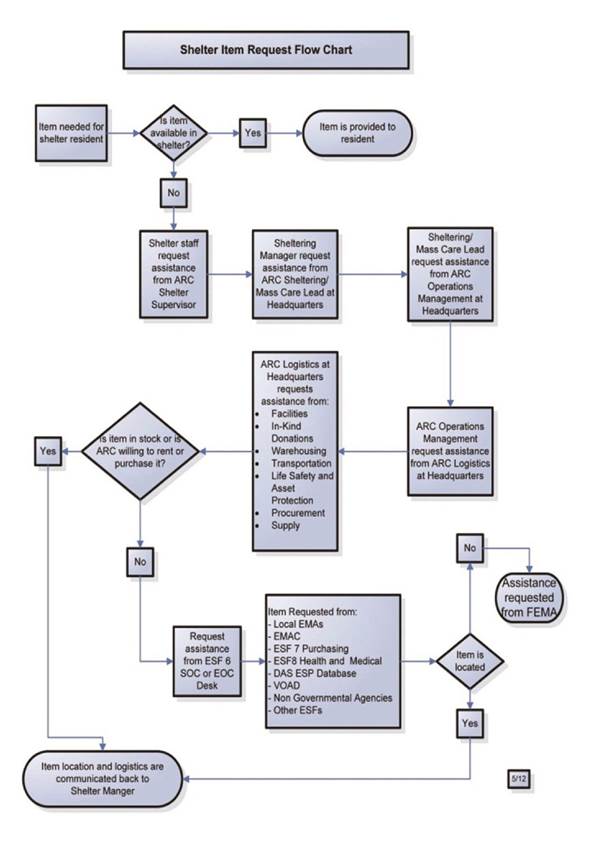
American
Red Cross Process for Requesting FNSS Resources
4) Functional Needs
Support Services and Resources
·
General
Resources
·
Durable
Medical Equipment (DME) Resources
·
Consumable
Medical Supply (CMS) Resources
·
Pharmacy
Support Services
·
Personal
Assistance Services (PAS) Resources
·
Communication
Tools for Individuals with Limited English Proficiency
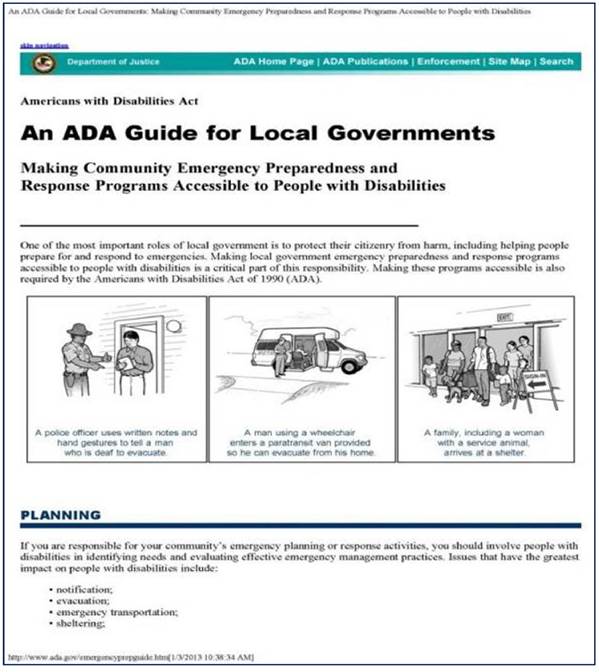
The Stafford Act and the Post-Katrina
Emergency Management Reform Act (PKEMRA), along with Federal civil rights laws,
mandate integration and equal opportunity for people with disabilities in
general population shelters. The Americans with Disabilities Act of 1990 (ADA),
the Rehabilitation Act of 1973, and the Fair Housing Act (FHA), regulations and
agency guidance, as well as state counterparts, define the scope
responsibilities.
Legal References
·
ADA
Best Practices Tool Kit for State and Local Governments, Chapter 7, Emergency
Management under Title II of the ADA (2007), Addenda 1-3, and the Introduction
to Appendices 1 and 2 (Attached as Exhibit 1); Titles II, III, and V of the
Americans with Disabilities Act of 1990, 42 U.S.C. §§ 12101- 12103,
12131-12134, 12181-12188, and 12201-12213, as amended by the ADA Amendments Act
of 2008. Nondiscrimination on the Basis of Disability in State and Local
Government Services, 28 C.F.R. pt. 35. Nondiscrimination on the Basis of
Disability by Public Accommodations and in Commercial Facilities, 28 C.F.R. pt.
36. The Americans with Disabilities Act Title II Technical Assistance Manual
(1993) and Supplement (1994). The Americans with Disabilities Act Title III
Technical Assistance Manual (1993) and Supplement (1994).
·
Section
504 of the Rehabilitation Act of 1973, 29 U.S.C. §§ 794, as amended. Enforcement
of Nondiscrimination on the Basis of Handicap in Programs or Activities
Conducted by the Federal Emergency Management Agency, 44 C.F.R. pt. 16.
Enforcement of Nondiscrimination on the Basis of Handicap in Programs or Activities
Conducted by the Department of Justice, 28 C.F.R. pt. 39. Nondiscrimination on
the Basis of Handicap in Programs or Activities Receiving Federal Financial
Assistance, 45 C.F.R. pt. 84 (Department of Health and Human Services).
Nondiscrimination on the Basis of Handicap in Programs or Activities Receiving
Federal Financial Assistance, 34 C.F.R. pt. 104 (Department of Education).
Nondiscrimination Based on Handicap in Federally Assisted Programs and
Activities of the Department of Housing and Urban Development, 24 C.F.R. pt. 8.
·
Title
VIII of the Civil Rights Act of 1968 ("Fair Housing Act"), as
amended, 42 U.S.C. §§ 3601-3631. Discriminatory Conduct Under the Fair Housing
Act, 24 C.F.R. pt. 100.
·
The
Architectural Barriers Act of 1968, as amended, 42 U.S.C. §§ 4151-4157. Construction
and Alteration of Public Buildings, 41 C.F.R. pt. 101-19.
·
The
Homeland Security Act of 2002, 6 U.S.C. §§ 101-557, as amended.
·
The
Robert T. Stafford Disaster Relief and Emergency Assistance Act, 42 U.S.C. §§
5121-5206, as amended. Federal Disaster Assistance, 44 C.F.R. pt. 206.
·
The
Post-Katrina Emergency Management Reform Act, 6 U.S.C. § 761(d), as amended.
Emergency managers and shelter planners are
encouraged to investigate their applicable state laws and regulations.
Federal Laws Prohibiting Discrimination in
Emergency Programs on the Basis of Disability
·
Americans
with Disabilities Act of 1990
·
Stafford
Act of 1988
·
Rehabilitation
Act of 1973
·
Fair
Housing Act Amendments of 1988
·
Architectural
Barriers Act of 1968
·
Individuals
with Disabilities Education Act of 1975
·
Telecommunications
Act of 1996
Each provides affirmative obligations and
prohibitions of discrimination on the basis of disability.
No state or local government, or its
contractors, in providing services may, by law, policy or contract, provide
services below these standards without violating federal law.
The State of Georgia Functional Needs
Support Services Definition Document was created in order to provide a basic
understanding of the functional, access and medical needs of populations for
consistent future planning purposes in Georgia. The FNSS workgroup included the
Georgia Department of Public Health, the Georgia Department of Human Services,
the American Red Cross, the Georgia Emergency Management Agency, the Georgia
State Financing and Investment Commissions- State ADA Coordinator's Office and
the Georgia Department of Behavioral Health and Developmental Disabilities.
In early 2012, state agencies were getting
reports from locals about inconsistent messaging and planning related to FEMA
and State FNSS guidance and requirements. To address these concerns, to provide
clear and concise messaging and to present a unified approach, ESF 6 and 8 partners
formed the State FNSS Working Group. The work group developed a
Georgia-specific FNSS definition and presented this definition to local
partners in May 2012. Once the definition was established, shelter placement
guidance and planning considerations were developed. The official definition,
titled: State of Georgia Definitions. Functional and Access Needs and
Medical Needs Populations is as follows:
Individuals with functional and access
needs include (but are not limited to) people that have physical, sensory,
mental health, and cognitive and/or intellectual disabilities affecting their
ability to function independently without assistance. Others who may have functional
needs include older adults, women in late stages of pregnancy and individuals needing
bariatric equipment. The general assumption is that most persons with
functional needs can function perfectly well in a general population shelter
with proper support. An additional assumption is that the person with the
access or functional need has the right to self-determination, whenever
possible. Self-determination is a practice that asserts that the individual has
the right and ability to assess their own needs, receive education about their
options and be involved in the decision making process. With the proper
support, individuals with functional and access needs benefit equally from the
services provided in general population shelters, and should almost always be
housed in those shelters.
Functional Needs Support Services (FNSS)
are defined as services that enable individuals to maintain their independence
in a general population shelter. FNSS includes:
·
Reasonable
modification to policies, practices, and procedures
·
Durable
medical equipment (DME)
·
Consumable
medical supplies (CMS)
·
Personal
assistance services (PAS)
·
Other
goods and services as needed
Planning for FNSS in general population
shelters includes the development of mechanisms that address the needs of
children and adults in areas such as:
·
Ability
to access temporary shelter facilities
·
Communication
assistance and services when completing the shelter registration process and
other forms or processes involved in applying for emergency-related benefits
and services including federal, state, tribal and local benefits and services
·
DME,
CMS, and/or PAS that assist with the activities of daily living and individuals
requiring accommodations specific to their condition are also encouraged to
take their own supplies to the shelter
·
Access
to medications to maintain health, mental health and function
·
Available
sleeping accommodations (e.g., the provision of universal/accessible cots or
beds and cribs; the placement, modification, or stabilization of cots or beds
and cribs; the provision and installation of privacy curtains)
·
Access
to orientation and way-finding for people who are blind or have low vision
·
Assistance
for individuals with cognitive and intellectual disabilities
·
Auxiliary
aids and services necessary to ensure effective communication for persons with
communication disabilities
·
Access
to an air-conditioned and/or heated environment (e.g., for those who cannot regulate
body temperature)
·
Refrigeration
for medications
·
Availability
of food and beverages appropriate for individuals with dietary restrictions
(e.g., persons with diabetes or severe allergies to foods such as peanuts,
dairy products and gluten)
·
Providing
food and supplies for service animals (e.g., dishes for food and water, arrangements
for the hygienic disposal of waste, and portable kennels for containment if
requested)
·
Access
to transportation for individuals who may require a wheelchair-accessible vehicle,
individualized assistance and the transportation of equipment required in a shelter
because of a disability
·
Assistance
locating, securing, and moving to post-disaster alternative housing, which
includes housing that is accommodating to the individual's functional support needs
(e.g., accessible housing; housing with adequate space to accommodate DME; or
housing located in close proximity to public transportation, medical providers,
job or educational facility, and/or retail stores)
·
Assistance
with activities of daily living such as:
o
eating
o
taking
medication
o
dressing
and undressing
o
transferring
to and from a wheelchair or other mobility aid
o
walking
o
stabilization
o
bathing
o
toileting
o
communicating
·
Children
and adults with and without disabilities who have access or functional needs
who require medical services may not be excluded from a general population shelter.
Plans should direct that, at a minimum, medical care that can be provided in the
home setting (e.g., assistance in wound management, bowel or bladder management,
or the administration of medications or use of medical equipment) is available
to each general population shelter.
MEDICAL NEEDS POPULATIONS
·
Individuals
who are not self-sufficient or who do not have adequate support from
caregivers, family, or friends may need assistance with managing unstable, terminal
or contagious conditions that require observation and ongoing treatment; managing
intravenous therapy, tube feeding, and vital signs; receiving dialysis, oxygen,
and suction administration; managing wounds; and operating power dependent
equipment to sustain life. These individuals require support of trained medical
professionals.
Note: Persons with functional or medical
needs have typically exhausted all other resources (family, neighbors, public
transportation, etc.) and still need assistance for evacuation and/ or
sheltering before, during, and possibly after a disaster or emergency. These
individuals typically reside in single homes or multiple family dwellings in
the state and are not residents of hospitals, residential health care
facilities, or any community-based residences or services that are already
subject to emergency planning requirements.
One of the first questions most emergency
managers and planners ask is "Where do we start?" This is a good question,
and while the answer to this question could be as varied as the community being
planned for, this section includes some tips and strategies for beginning FNSS
Planning. Regardless of the starting point, the mindset should be for including
the whole community in planning.
This means:
·
Understanding
and meeting the needs of the entire affected community
·
Engaging
partners of the community (public, private, and civic sectors) in defining IFAN
needs of your community and devising ways to meet them
·
Strengthening
the assets, institutions, and social processes that work with IFAN on a daily
basis to improve resilience and emergency management outcomes
This section includes six steps for FNSS
Planning that are indicative of whole community planning including:
Step
1: Complete an Emergency Planning Assessment
Step
2: Identify Potential Mass Care Partners
Step
3: Review and Analyze IFAN Statistics for the Community
Step
4: Identify and Invite IFAN Partners to the Planning Table
Step
5: Identify FNSS Resources for Planning
Step
6: Special Considerations to Effectively Include IFAN in Emergency Planning
Note: While a majority of this section
focuses on shelter planning for people with functional and access needs, these
concepts can be applied to each phase of the emergency management cycle
(preparedness, planning, response, recovery and mitigation).
Review your current plans, processes and
procedures to see if they include Functional and Support Services. Identify any
gaps within current plans and keep in mind compliance with the Americans with
Disabilities Act (ADA) requirements.
The Americans with Disabilities Act (ADA)
requires shelters to afford equal access to all shelter services including (but
not limited to) safety, food, services, comfort, information, a place to sleep
(until it is safe to return home), and the support and assistance of family,
friends, and neighbors.
Look at where you are, identify gaps, and
identify what your current plans do. ADA is not just applicable to architecture
issues.
Start with an assessment of your current
plans and standard operating procedures, and ask the following questions:
·
Do
you have a process for input from IFAN, agencies and community based organizations
representing IFAN in all phases of your emergency planning? These
agencies/organizations include, but are not limited to, those that address
preparation, notification, evacuation, transportation, sheltering, medical and
social services, temporary lodging and/or housing, clean-up, and remediation.
·
Do
you seek input and participation from IFAN when you conduct exercises and
otherwise test your preparedness?
·
If
you have a contract or other arrangement with any third party entities, (i.e.,
the American Red Cross, a volunteer agency or other local government) to
provide emergency planning and/or emergency management or response services,
does your contract or other documentation of your arrangement contain policies
and procedures to ensure that the third party entities comply with ADA
requirements?
If you have identified any gaps in your
plans and processes, then consider working with your key partners on
identifying community resources.
Once the initial planning assessment is
complete, the next step will be to identify additional stakeholders. The core
mass care planning partners include:
·
Emergency
Management Agencies
·
American
Red Cross Chapters
·
Department
of Human Services, Division of Family and Children Services
·
District
Public Health Offices
·
Area
Agencies on Aging
Below are examples of
agencies/organizations at the local level that should be included in Emergency
Support Function 6 planning for Functional Needs Support Services (FNSS), as
well as potential roles and responsibilities for each of the partners.
A place to start for this step is the
existing Local Emergency Operations Plan (LEOP). Within the plan, EMA Directors
identify partner agency roles and responsibilities for inclusion in the LEOP
for each Emergency Support Function.
Following are some examples of potential
partner organizations and agencies which may be available at the local, county,
regional or district office level:
·
ADA
Coordinator's Office
·
Regional
Healthcare Coalitions
·
Behavioral
health and developmental disabilities partners
·
Local
advocacy groups for individuals with functional and access needs
·
Other
non-governmental organizations including faith based organizations
·
Civic
clubs and organizations
·
Local
leadership
·
Transportation
service providers
·
Law
enforcement
·
Others
as determined by local jurisdiction
Within the State of Georgia, Department of
Human Services (DHS) is the lead state coordinating agency for ESF 6, Mass
Care. The American Red Cross is the lead voluntary agency for sheltering within
the state. Knowledge of ESF 6 roles and responsibilities are key in overall
FNSS planning considerations. Planning for FNSS should be incorporated into all
phases of the emergency management cycle and should address shelter operations.
The following are some examples of ESF 6
Partner roles and responsibilities.
Human Services/American Red Cross
·
Coordinate
the planning for FNSS for all phases of the emergency management cycle,
specifically in shelters.
·
Coordinate
with mass care partners to identify and provide alternate facility options for
individuals unable to remain in shelters (e.g., hotel or personal care home). A
list of community living options to utilize during the recovery phase of a
disaster is available in the appendix.
·
Integrate
local advocacy groups and organizations that provide services to individuals
with disabilities and/or functional and access needs into FNSS planning. These
groups can assist in identifying the types of disabilities and/ or functional
and access needs that are present in the community.
·
FNSS
shelter planning.
·
Identify
local resource providers of FNSS and, if possible, assist with the establishment
of a Memorandums of Understanding (MOUs) or other agreements to provide FNSS
resources to shelters if needed.
·
Participation
on Community Organizations Active in Disasters (COADs), Citizens Corps
Councils, Local Emergency Planning Committees (LEPCs) and Medical Reserve Corps
or community coalitions, and encourage the development of FNSS sub-committees
to ensure whole community planning.
o
Note:
one way to engage community partners is to identify and participate in existing
community coalitions to avoid duplication of resources.
Aging Services
·
Establish
relationships with Area Agencies on Aging (AAAs) to pre-identify areas within
communities with large groups of older adults that may need transportation or
other types of assistance during a disaster.
·
Identify
and include representatives from groups and organizations that represent the
interests of older adults for FNSS in general shelters.
·
Identify
the types of FNSS that may be needed to support older adults within the
community.
·
Establish
agreements with equipment and service providers based on determined needs.
·
Behavioral
Health and Developmental Disabilities (Mental Health)
·
Identify
and invite local and/or regional mental health providers to participate in FNSS
planning.
·
Provide
assistance with identifying local mental health resources specific to the
community that may be needed to support FNSS.
·
Establish
agreements with providers to offer these resources in shelters and as the need
arises.
Public Health
·
Identify
alternate facilities that can accommodate individuals determined
·
to
have needs that cannot be met in a general population shelter. Alternate facilities
should be chosen based on the degree of need for each individual and should be
the "least restrictive" option possible depending upon that need.
·
Establish
agreements or MOUs with alternate facilities prior to an event and coordinate
with local EMA and ARC to provide transportation for these individuals from the
shelter to the alternate facility.
·
Work
with ESF 6 Partners to identify Functional Needs Support Services locally and
assist with building the needed relationships to access these resources to
support shelter operations.
·
Coordinate
healthcare staffing (primarily Registered Nurses) for FNSS, to assist with
routine healthcare assessments, as requested by the FNSS Manager. All
emergencies are handled by the local Emergency Medical Services provided,
through "911" or designated emergency number.
Emergency Management
·
Support
ESF 6 Coordinator and provide overall coordination of disaster response and
recovery.
·
Develop
communication plans and procedures to ensure all mass care partners are
included in the planning process and have been trained on their roles and
responsibilities in accordance with the LEOP.
·
Develop
communication plans with mass care agencies/organizations at the state level to
support local operations if the need arises.
Georgia Department of Agriculture (GDA)
·
Provides
support to shelter operations through the provision of food and other necessary
items for service dogs.
·
Identifies
and coordinates the location of pet friendly shelters near shelters to allow
evacuees to care for their pets during disasters.
·
Supports
DHS and ARC in the provision of food and food services for shelters upon
request.
Georgia Volunteer Organizations Active in Disasters (GAVOAD)
·
Provides
various services to support shelter operations such as child care assistance,
feeding and other support.
·
Provide
assistance with recovery services after a disaster to help individuals regain
their independence and return to, or as close as possible to, their pre- disaster
standard of living.
·
Provides
assistance to individuals, families and local communities with additional
support and services not related to shelters such as debris clearance, managing
volunteers and donations, establishment Long Term Recovery Centers (LTRCs),
etc.
IFAN are a diverse group. Complex
variations in the health status, living environments, and social situations of
those with functional and access needs make it hard to plan for this population
during emergencies.
For example, older adults are at increased
risk of disease and death during emergencies because of factors such as the
following:
·
A
higher prevalence of chronic conditions, physical disability, cognitive impairment,
and other functional limitations
·
Dependence
on support systems for medical care, medication, food, and other essential
needs
·
Potential
limitations in their mobility, their access to transportation, or other aspects
of functional autonomy
Emergencies also can disrupt the support
systems on which many IFAN rely. For many IFAN, independent living is made
possible only with help from friends, family, and in-home services that provide
meals, home-based health care, and assistance with chores and personal care
needs. If some IFAN are not able to get the medications, equipment, or special
care they need they can be at increased risk of complications and death during
an emergency.
The majority (93%) of Medicare enrollees
aged 65 years or older live in the community, rather than in nursing homes or
other congregate settings. Nearly one- third of this group lives alone.1
Note: Since whole community planning is at
times an overwhelming task, Step 3 focuses on shelter planning for individuals
with disabilities. Each step can be applied to other vulnerable populations
identified within your community for a whole community approach.
STRATEGIES AND OPTIONS FOR IDENTIFYING IFAN
The ability to identify which IFAN will
have a functional or access requirement during an emergency is a primary
obstacle to helping those in need during a crisis situation.
Among the many potential approaches for
identifying IFAN populations for preparedness planning, the following three
methods may assist planners:
1. Characterizing the
population
2. Using Geographic
Information Systems (GIS)
3. Building, using,
and maintaining registries
1
ref: Federal Interagency Forum on Aging-Related Statistics. Older Americans
2010: Key Indicators of Well-Being. Washington, DC: U.S. Government Printing
Office; 2010. www.agingstats.gov/agingstatsdotnet/Main_Site/Data/2010_Documents/Docs/OA_2010.pdf.
Characterizing the Population
Officials at all jurisdictional levels need
to understand the basic epidemiologic characteristics of the different
populations encompassed in the IFAN. Epidemiologic data can be used to plan the
delivery of services, medications, durable medical equipment and other
materials needed to support this population during all phases of an emergency.
For example, data that indicates a high prevalence of diabetes in a particular
community can lead to more comprehensive stockpiling and planning for
distribution of insulin during an emergency. Other categories of information
that can help jurisdictions develop preparedness plans include:
·
Demographic
characteristics, including the number of older adults and their age, sex, and
race/ethnicity, as well as the size and types of cultural subgroups
·
Prevalence
of chronic medical and behavioral health conditions, disabilities and functional
limitations
·
Prevalence
of chronic conditions that require specific medications, durable medical
equipment or special medical care
·
Primary
language and other languages spoken by significant portions of the population
·
The
proportion of older adults who live in the community and the ratio that live in
independent living, assisted living or long-term-care facilities
·
Residency
patterns, including those that are permanent, seasonal or periodic
·
The
percentage of older adults who receive services through organizations such as
the Aging Services Network, social service agencies or home health agencies and
the proportion of community-dwelling adults who do not receive services from
any organizations
Potential sources for these data include
the following:
·
Community
surveys
·
Disease
registries
·
Hospital
discharge databases
·
Medicaid
and Medicare databases
·
U.S.
Census
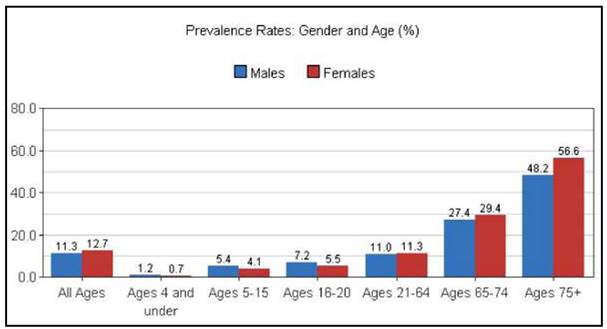
After the initial planning assessment and
identification of potential stakeholders, the next step is to review data
specific to your community in order to identify who lives in the community and
their needs. According to the 2010 US Census, approximately 12.1% of the
population in Georgia is considered to have a disability. This means that
within Georgia, there are approximately 1.2 million individuals with some type of
disability. The majority (38.2%) of these persons are 65 years and older (Table
1), and the prevalence rate increases in those 75 years and older (Figure 1).
Table 1: State of Georgia
Disability Characteristics
|
Subject
|
Total Population
|
Estimated Number
of People With A Disability
|
Percentage of Population
with A Disability
|
|
Total population*
|
9,619,740
|
1,161,966
|
12.1%
|
|
Age Distribution of Persons with
Disabilities
|
|
under 5 years
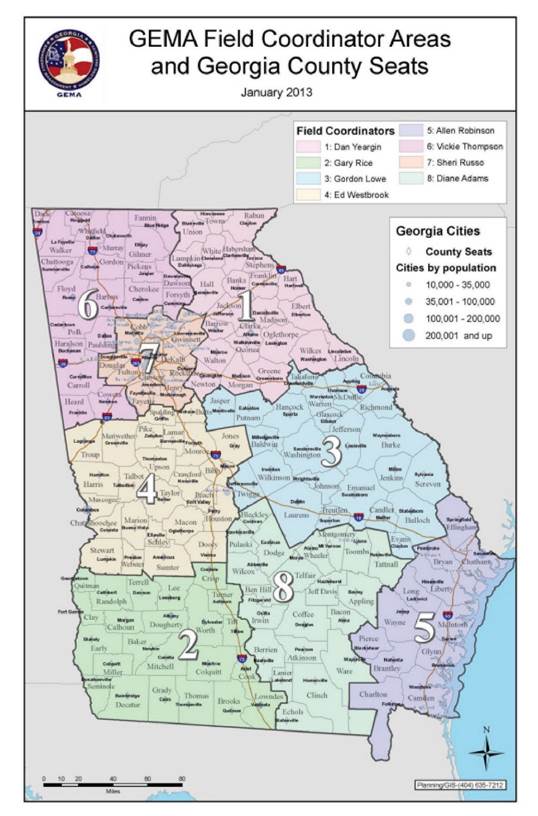
|
673,981
|
7,461
|
1.1%
|
|
5 to 17 years
|
1,810,734
|
91,189
|
5.0%
|
|
18 to 64 years
|
6,088,938
|
663,904
|
10.9%
|
|
65 years and
over
|
1,046,087
|
399,412
|
38.2%
|
*
Civilian, non-institutionalized population Source: 2010 US Census, American
Fact Finder
(http://factfinder2.census.aov/faces/nav/isf/paaes/searchresults.xhtml?refresh=t)
Figure 1: The prevalence of disability
among non-institutionalized people by gender and age group in Georgia, 2011
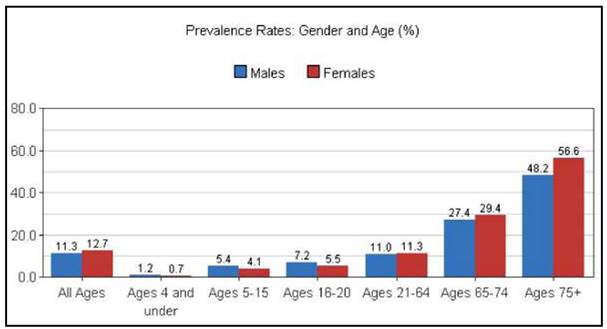
Ref:
www.ilr.cornell.edu/edi/disabilitystatistics. abstracted 2013
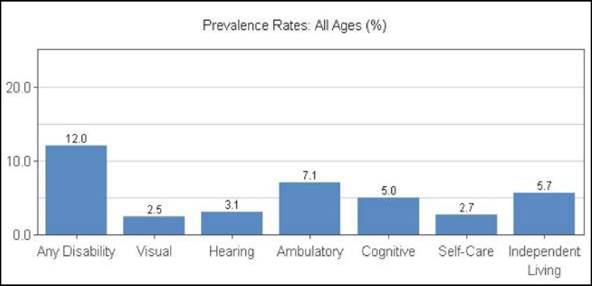
Note: Gaining an understanding of not only
the number but the types of disabilities these data represent will help in
planning for IFAN. The following figure provides a breakdown of the above data
by type of disability.
Figure 2: Prevalence of disability among
non-institutionalized people of all ages in Georgia in 2011
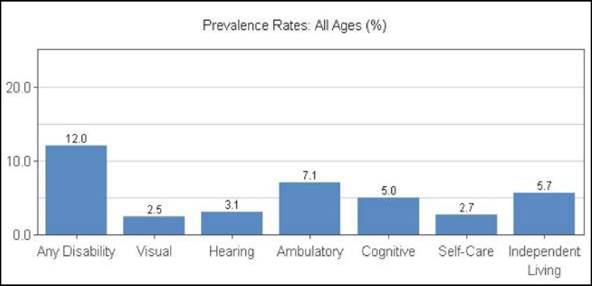
Ref: www.ilr.cornell.edu/edi/disabilitystatistics,
abstracted
2013
Note: In planning for Functional Needs
Support Services (FNSS), it is important to understand that each disability is
based upon a spectrum or level of disability and not all persons with
disabilities will need FNSS during an emergency.
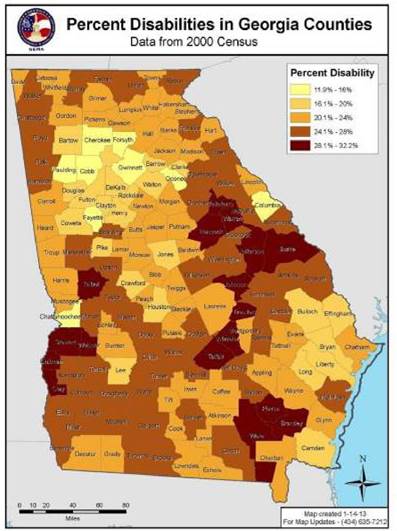
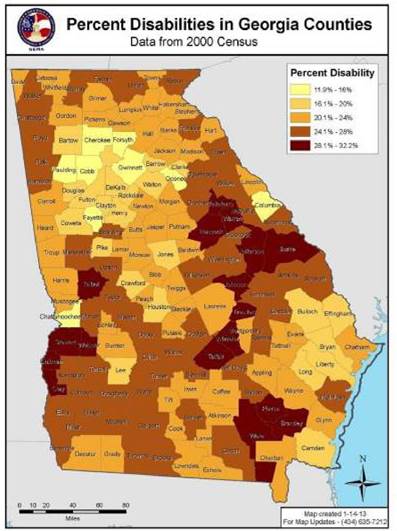
Using Geographic Information Systems (GIS)
Many emergency managers are now using (GIS)
mapping to locate concentrations of functional needs populations within their
communities. Figure 3.0 geographically depicts percentages of individuals with
disabilities by county using Geographic Information System (GIS) mapping tools.
When using mapping resources to identify
concentrations of individuals with disabilities, or individuals with functional
and access needs, there are several factors to consider when interpreting and
displaying the data including:
1) What is your
ultimate goal for use of the data?
2) How can the data be
represented in a way that will enable users to better allocate resources?
3) What types of other
variables (i.e., hazards) significantly impact local capabilities for providing
assistance to individuals with disabilities, or individuals with functional and
access needs.
GIS relies on special software and
available data to pinpoint geographic areas where individuals with disabilities
are likely to live. Utilizing GIS to develop maps where individuals most likely
reside can help emergency responders and disability service providers during a
disaster know which areas may need priority attention or special consideration.
GEMA offers a Georgia-specific mapping tool
called GO DAWGS-the Georgia Online Disaster Awareness Geospatial System. GO
DAWGS is a web based geospatial visualization tool that allows the State
Operations Center (SOC) to display information in relation spatially, creating
a Common Operating Picture that Emergency Responders may use to assist them in
drastically improving the situational awareness of response, recovery and
coordination to both natural and man-made disasters. https://godawgs.gema.ga.gov
Figure 3 provides a visual image of
disability by county within Georgia. The 12.1% overall average for the state
includes those counties with fewer persons with disabilities, as well as those
counties who have over 28% of their population with some type of disability.
Note: These higher percentages may represent counties with a larger elderly
population.
FIGURE 3: Percent of Georgia Population
with Disabilities by County
It is vitally important to understand the
local disability demographics (e.g., large concentrations of citizens with
disabilities and senior housing communities). Most people with disabilities
live and work independently and are dispersed among the population. To
accurately plan, it is important to have a solid understanding of community
demographics. Data on local city and county disability characteristics are
limited. For this reason, it is suggested that local emergency managers use
this information only as a guideline for predicting functional and access needs
within their communities.
Note: Users of this guide are encouraged to
investigate the needs of their local communities more thoroughly. To obtain
local, regional, statewide and national data, local officials should work with
local disability service providers and city/county planning departments.
Where To Go For Disability Data:
Note: There are many databases with
information on individuals with disabilities; however the federal database
provides a standard which can be used throughout the state and region. These
data can be applied to your community population to get a broad estimate of how
many persons within your community may have a functional and/or access need
during an emergency. However, local agencies and non-governmental organizations
may have information which better represents your community.
U.S. Census Bureau
The definition of a disability varies,
therefore, the collection of disability statistics depends on the purpose for
which it is being used and the survey collecting the information. The Census
Bureau collects disability data from four surveys; however, other agencies also
collect disability data. Depending on your needs, one survey may be more
suitable than another. For more information, please visit www.census.gov/hhes/www/disability/disability.html.
The American Community Survey (ACS)
ACS is part of the National Center for
Health Statistics since 2005, annually surveys American households on various
demographic and socioeconomic parameters and disability data.
http://www.census.gov/acs/www/about
the survey/american community survey/
The ACS replaced the decennial census
long-form in 2010 and collects long-form-type information throughout the
decade, rather than only once every 10 years. The ACS data provides a
continuous stream of updated information for states and local areas.
Limitations of ACS data in Georgia:
·
ACS
is an ongoing survey of persons who reside in counties with a population great
than 65,000. This means that there currently no specific data available for
rural counties within Georgia. However, in the near future, ACS survey 5-year
averages will be used to provide data estimates of all Georgia counties.
·
Also,
since the ACS is a household survey, people living in institutions such as nursing
homes are not included.
To help with specific information on
populations with disabilities, there are several websites that have taken the
ACS data and made it more accessible for planners. Several of these sites are
listed below.
American FactFinder
Provides access to data about the United
States, Puerto Rico and the Island Areas. The data in American FactFinder come
from several censuses and surveys. A guided tour of these data is available at http://factfinder2.census.aov/faces/nav/isf/paaes/index.xhtml.
Disability Statistics.Org
This Cornell University website uses
several data sources, including Current Population Survey, Census 2000 and the
American Community Survey (ACS) to provide state-specific data on disability. http://www.disabilitystatistics.org/
Personal Assistance Service Center
The Center for Personal Assistance Services
has compiled state and national data on the prevalence of overall disability
and of self-care difficulty, by gender, age, race and ethnicity, type of
disability, family income, recipient benefit, employment status and living
arrangement. These statistics are based on tabulations from the 2009 American
Community Survey (ACS) and provide county disability information for non-rural
Georgia counties.
http://www.pascenter.org/state
based stats/disability stats/acs
counties.php?state=georgia&title=Populations+with+Disabilities%3A+Counties
Identifying at-risk populations within
your community: Resources
There are many online resources with regard
to at-risk populations. The following is a workbook and an eTool developed by
the CDC to help walk you through the process of identifying and working with
the at-risk population within your community.
PUBLIC HEALTH WORKBOOK to Define, Locate,
and Reach Special, Vulnerable, and At-Risk Populations in an Emergency
http://www.bt.cdc.gov/workbook/pdf/ph
workbookFINAL.pdf
This document describes a process that will
help planners to define, locate, and reach at-risk populations in an emergency.
Additional tools are included to provide resources for more inclusive
communication planning that will offer time-saving assistance for state, local,
tribal, and territorial public health and emergency management planners in
their efforts to reach at-risk populations in day-to-day communication and
during emergency situations.
If you follow the process outlined in this
document, you will begin to develop a Community Outreach Information Network
(COIN)-a grassroots network of people and trusted leaders who can help with
emergency response planning and delivering information to at-risk populations
in emergencies. Building a strong network of individuals who are invested in
their community's well-being, who are prepared and willing to help and who have
the ability to respond in an emergency is just the start. You must also include
network members in your emergency preparedness planning, test the capacity of
your COIN to disseminate information through preparedness exercises and make
changes to your preparedness plans based on the evaluation of those exercises.
The At-Risk Population's eTool is a
companion to the above cited workbook:
http://www.orau.gov/SNS/AtRiskTool/
This tool will help you create a Community
Outreach Information Network (COIN) to reach at-risk populations within your
community in an emergency. It provides information and tools on creating a
Community Outreach Information Network (COIN) for more efficient information
distribution to those populations. Navigating through the eTool is simple and
provides step by step information and planning tools.
Building, Maintaining and Using Registries
Note: The following section on registries
was developed by the CDC and is included in this document as a discussion of
several types of registries, as well as information on the resources needed to
develop and maintain a registry.2
In the context of emergency preparedness,
the purpose of a registry is to identify before an event occurs those
individuals who may need special attention or help before, during, or after an
emergency. Registries can be based on the specific type of help a person needs
(e.g., medical, transportation or other special needs), or they can be used for
the broader purpose of identifying any person who might need any type of help
during an emergency. Many jurisdictions also use registries as a way to provide
information to older adults on how to prepare for emergencies.
Three Types of Registries Include:
·
Special
needs registries
may have a broad scope, listing any person who might need help during an event,
or be limited to specific special needs (e.g., individuals with specific types
of physical or mental disability, impaired mobility, dependence on medication
or medical equipment or limited cognitive function).
·
Medical
needs registries
are limited to individuals who have specific, identifiable medical needs. These
registries may require documentation from a doctor about the person's specific
diagnosis and medical requirements (e.g., for oxygen, dialysis or other life
threatening disorders).
·
Transportation
registries
identify people who cannot evacuate a location or area before an event without
help (e.g., older adults, people with special or medical needs).
Development, Maintenance, and Resources
Local registries are often the product of
collaborations between government entities, community groups and social service
providers. In some jurisdictions, registries are developed and maintained by a
local or state government entity, such as the Office of Emergency Management.
In areas where funding is limited (e.g., rural areas), groups may pool their
resources to develop regional registries.
To account for changes in place of
residence, special needs and other factors for people already registered, as
well as for incremental additions, registries must be updated regularly.
Keeping registries up-to-date is difficult because the number of potential
registrants is always changing as people visit or move into or out of a given
area.
Registry development and maintenance
requires sustained staffing and resources. Some jurisdictions fund registries
through emergency response funds, while others rely on volunteers and community
collaboration.
2
Identifying Older Adults and Legal Options for Increasing Their Protection
During All-Hazards Emergencies: A Cross-Sector Guide for States and Communities
Atlanta: U.S. Department of Health and Human Services; 2012.
Methods for collecting information on
registrants may include the following:
·
A
Web form individuals or their family/advocates can use to submit and update
their information
·
A
central phone number that people can call to register
·
Social
service workers or volunteers who collect information from clients when they
apply for other public health services
·
Direct-mail
registration forms that people can fill out and return
Liability
Jurisdictions may be concerned about
liability and about creating the expectation that, by enrolling an individual
into a registry, help is guaranteed. To address this concern, many
jurisdictions require that registrants be fully informed about the following:
·
With
whom the information will be shared
·
How
information will be used
·
Security
measures in place for protecting information
·
The
type of help that may be available
·
Limitations
on help (e.g., help is not guaranteed)
Effectiveness
Registries are used with varying degrees of
effectiveness and are influenced by factors such as geography, demographics,
perceived risks, requirements for updates and maintenance, and resource
allocation.
Communities should fully assess whether
registries are an efficient, effective way to identify their specific needs
population, and communities need to determine whether they can support and
maintain a registry with their existing resources.
Once emergency coordinators have conducted
a planning assessment, identified ESF 6 stakeholders and reviewed local
demographics, the next step is to invite representatives of the largest IFAN
communities to planning meetings. There are a variety of ways to incorporate
IFAN into the planning process. When considering who to invite to meetings, it
is important to have a good understanding of community demographics.
Gathering demographic information will be a
good starting point for understanding the areas of greatest vulnerability and
for identifying the best representatives from the disability community. Based
on the national average of the population with functional and access needs,
take the population of any community and divide by five (20%). The result
approximates the number of residents with functional and access needs in your
community. As seen on the Georgia map of percent disabilities by counties, some
communities will have a larger or smaller proportion of IFANs. Remember, as
valuable as statistics are as a planning tool, they only provide emergency
coordinators with an overview of the IFAN population within your community.
What is more important is the experience of the person with functional and
access needs. In planning, the following questions should be considered:
·
What
is it like to be a person with a disability during and after an emergency?
·
Can
warnings be heard or understood?
·
Can
the home or workplace be exited quickly?
·
Can
a person with an access need move about the community after evacuating?
·
Are
there necessary or even vital daily items (medicines, power supplies, medical
devices) that are not likely to be available in shelters?
·
Are
basic services, like restrooms and showers, available and accessible?
·
Does
the person require assistance from a caregiver?
These questions are not always easy to
answer. That is why it is imperative to analyze needs and form meaningful
partnerships with advocacy groups or persons with functional and access needs,
directly, to ensure planning is comprehensive.
Emergency managers can draw from community
representatives to establish an advisory committee on developing functional and
access needs support services (FNSS). The committee should consist of a
cross-section of community residents with disabilities and unique functional
needs, as well as, representatives from local emergency management agencies,
service provider organizations, advocacy groups and local government agencies.
An emergency manager has a variety of
choices for establishing an advisory committee on emergency preparedness for
people with disabilities. Popular options include:
a)
Development
of a stand-alone committee
b)
Development
of a sub-committee as part of the local disaster planning group
c)
Development
of a committee as a component of the local Citizen Corps Council
Planners should keep in mind that having a
disability, either by birth, disease, age or accident, is part of the human
experience. Involving and listening to people with disabilities provides the
best insights for addressing their needs.
Emergency planners should:
·
Work
with disability service providers to identify those in the community who might
have functional needs ahead of a disaster or emergency. Doing so results in an
improved emergency plan, a better determination of resource needs and more
informed actions and decisions.
·
Customize
awareness and preparedness messages and materials for specific groups of people
and put them in alternative and accessible formats, thereby increasing the
ability of these individuals to plan and survive in the event of an emergency.
Such preparedness allows appropriate allocation of critical personnel,
equipment and assets during the response period, and it reduces 911call volume.
·
Educate
citizens with disabilities about realistic expectations of service during and
after an emergency, even while demonstrating a serious commitment
·
to
their functional needs. Such education results in a more cooperative relationship
with local authorities and enhances their appreciation of the concerns of
people with disabilities. It also leads to improved response by the entire
community.
·
Learn
and gain from the knowledge, experiences, and non-traditional resources the
disability community can bring to a partnership effort with emergency
professionals. By utilizing and embracing members of the disability community
as partners in the planning process, as well as in drills and exercises,
emergency personnel often discover creative solutions before they are needed.
These solutions may benefit not only the disability community but also the
general population. As mentioned earlier, the state has a coalition designed to
address disability-related issues in emergency management and to put together
inclusive plans. In addition, there are some good examples of local coalitions
within the state, including Gwinnett County, Clayton County, Macon-Bibb and
Augusta-Richmond County. These committees include emergency management, first
responders, disability organizations and advocates, and hospital associations.
·
Work
with institutional and industry-specific groups that are not typically considered
emergency service resources, but that can offer valuable and timely support to
emergency professionals. Identifying these groups ahead of time will lead to a
better prepared service community that is able to take on responsibilities
during an emergency. It also leads to a unified team able to quickly assess and
communicate service gaps during an emergency. Examples include Durable Medical
Equipment and Consumable Medical Supplies service providers and independent
living centers.
·
Use
local Community Emergency Response Teams (C.E.R.T.) to engage and train
individuals from the disability community. Local jurisdictions are encouraged
to actively recruit persons with disabilities to serve on CERT teams in order
to meet FNSS requirements in your jurisdictions.
Note: The most effective way to view
emergencies through the eyes of people with disabilities is to involve
community members with disabilities in the planning and preparation process,
including drills and exercises.
Individuals with disabilities have
differing capabilities, opinions, needs, and circumstances, and no one
individual or organization speaks for all people with disabilities.
There are a variety of existing resources
available to local coordinators and responders seeking to include people with
disabilities in emergency management programs. It is not necessary to
"reinvent the wheel"; emergency managers should seek to tap into
existing partnerships to maximize efforts. Many groups already work with
government and civic officials to ensure that people with and without disabilities
work harmoniously on issues of common concern. Some common categories of
representation are government organizations, non-governmental organizations,
associations and institution participants, advocacy groups, local groups
serving specific and general disability populations, and volunteer organizations.
Government Organizations
Usually, the best place to start in selecting
and involving disability representatives is the local ADA Coordinator, the
disability agency or task force within the county commissioner or mayor's
office. If a public entity has 50 or more employees, it is required to
designate at least one responsible employee to coordinate ADA compliance.
Typically, officials in these organizations can assist in identifying a
cross-section of disability representatives within the community. Following is
a breakdown of the various organizations and agencies that represent the
interests of individuals with disabilities and/or functional and access needs.
Links to these organizations can be found on the State ADA Coordinator's
website (http://ada.georgia.gov/emergency-preparedness) under Emergency Preparedness.
State of Georgia Agencies
·
Georgia
State Financing & Investment Commission- State ADA Coordinator's Office
·
Department
of Human Services-Division of Aging Service
·
Department
of Human Services-Office of Facilities and Support Services
·
Georgia
Department of Behavioral Health and Developmental Disabilities
·
Georgia
Department of Public Health
·
Southeast
ADA Center
·
Georgia
Department of Community Health Refugee
·
Governor's
Council on Developmental Disabilities
·
Local
Americans with Disabilities Act Coordinator for city, county and universities
·
Local
Independent School Districts that provide services and resources to children
with disabilities.
Non-Governmental Organizations
·
American
Red Cross-Atlanta
·
Friends
of Disabled Adults & Children (FODAC)
Associations and Institution Participants
·
Center
for Advanced Communications Policy - Georgia Institute of Technology
·
Tools
for Life - The Alternative Media Access Network - Georgia Institute of Technology
Enterprise Innovation Institute
·
Atlanta
Alliance on Developmental Disabilities
·
Georgia
Association of the Deaf, Inc.
·
Brain
Injury Association of Georgia
·
Cystic
Fibrosis Foundation - Georgia Chapter
·
Epilepsy
Foundation of Georgia
·
Georgia
Association for Prader-Willi Syndrome
·
Institute
on Human Development and Disability
·
Shepherd
Spinal Center
·
Spina
Bifida Association of Georgia, Inc.
·
Additional
examples of associations and institutional partners are:
o
Representatives
from the home-based care industry, such as the local Visiting Nurse Service and
the Home Health Aides Association
o
Residential
healthcare facilities, such as nursing homes, skilled care homes and assisted
living facilities
Advocacy Groups
It is important to include representatives
from advocacy groups in the disability community, such as:
·
Access
Center for Independent Living
·
AID
Atlanta, Inc.
·
AIDS
Alliance for Faith and Health
·
Georgia
Advocacy Office (GAO)
·
Disability
Connections
·
Disability
Link
·
Emory
Autism Resource Center
·
National
Alliance on Mental Illness (NAMI) - Georgia
·
Statewide
Independent Living Council of Georgia, Inc.
Local groups serving specific and general disability populations (e.g.,
people who are blind, deaf, or have limited mobility or cognitive disabilities)
·
GACHI,
Serving the Deaf and Hard of Hearing, local offices available
·
Georgia
Radio Reading Service (GaRRS)
·
Asperger
Syndrome Partners & Individuals Resources, Encouragement & Support
(ASPIRES)
·
Atlanta
School for the Deaf GA Parent/Infant Network/Education
·
Autism
Society of America - Greater Georgia Chapter
·
Bainbridge
Advocacy Individual Network, Inc. (BAIN)
·
Center
for the Visually Impaired
·
Families
of Autism/Asperger's Syndrome Care, Educate, Support (F.A.C.E.S.)
·
Families
of Children Under Stress (FOCUS)
·
Fragile
Kids Foundation
·
Georgia
ARC Network
·
Georgia
Mental Health Consumers Network (Consumers of MHDDAD Services)
·
Georgia
Parent Support Network
·
Georgia
Rehabilitation Outreach, Inc.
·
Jewish
Family and Career Services of Atlanta
·
Parent
to Parent of Georgia
·
Centers
for Independent Living (CILs)
·
Individuals
with disabilities who, though not affiliated with a group, are known to
emergency professionals and who are willing to participate in the planning
efforts
It is extremely important to select a range
of people in terms of both affiliation and disability. Involving people with
all major types of disabilities, including sensory, physical, mental, and
cognitive disabilities, as well as their caregivers, helps to establish the
most complete picture possible of the effect of disasters on people with unique
functional needs. A broadly based working group will be able to assist emergency
management planners in anticipating the true impact of the disaster on the
overall community. This leads to a more detailed, comprehensive and thoughtful response
plan for any community.
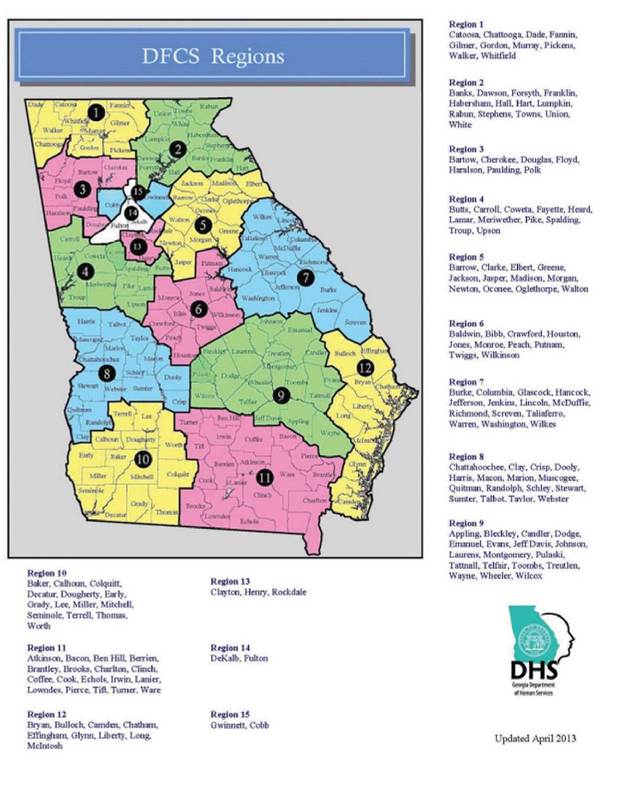
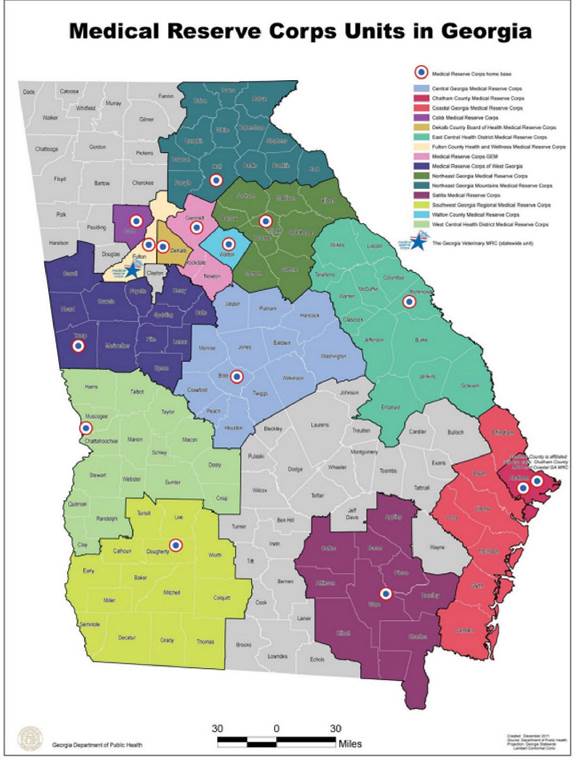
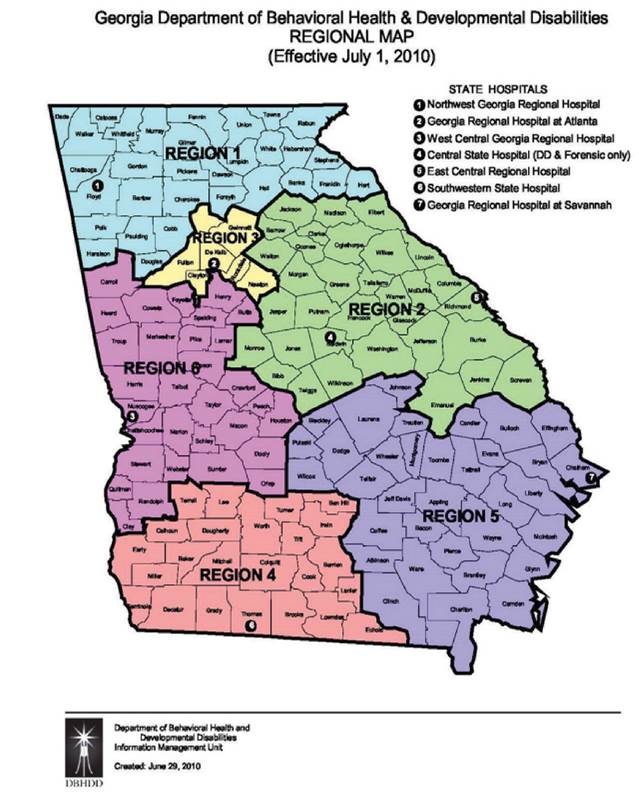
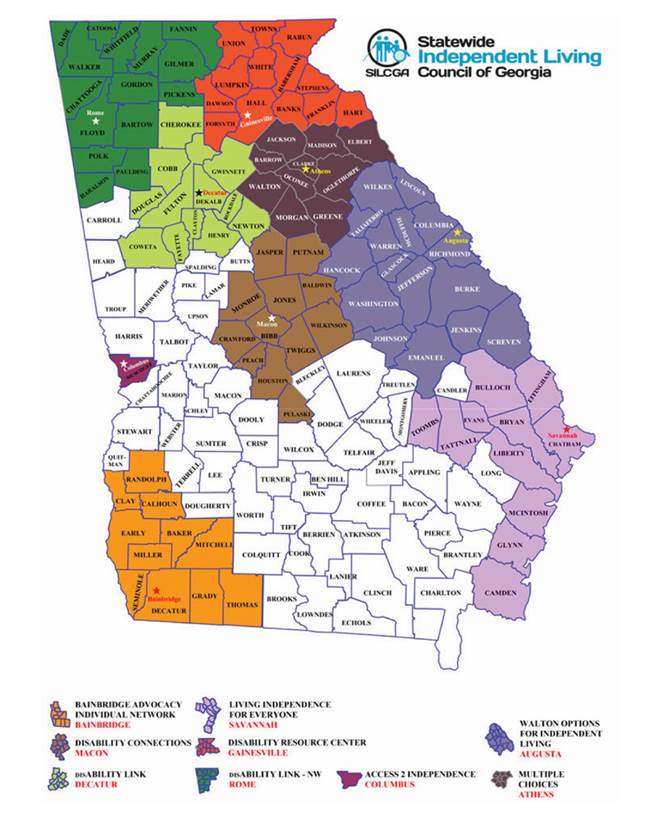
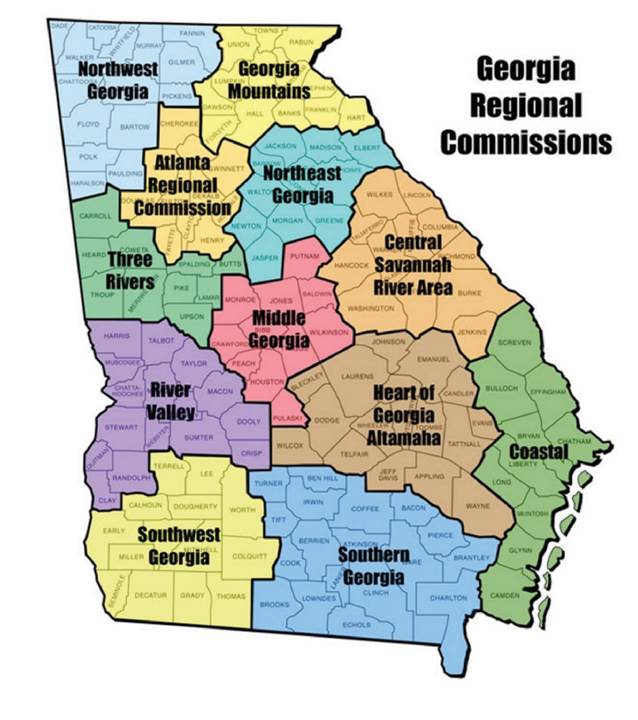
In addition to identifying potential
partners, it is helpful to understand service delivery areas for each agency or
organization. One tool that has proven to be very valuable is the use of
service delivery area maps for the various stakeholder and partner agencies.
These maps are available for reference in the appendix.
Each step mentioned is extremely important
for inclusion of people with disabilities in emergency management programs.
Completing an emergency planning assessment, identifying ESF 6 Stakeholders,
completing a disability data review and analysis, inviting disability
representatives to the planning table and maximizing existing resources are all
keys to successful collaboration. However, Step 6 is equally important and will
ensure long lasting successful partnerships with the disability community. It
is important to realize that people with disabilities, even more than other
demographic segments of the population, are not a homogeneous group. Remember,
the "disability community" is one that people can "join" at
any time.
Use People First Language (Language is
Important)
Positive language empowers. When writing or
speaking about people with disabilities, it is important to put the person
first. Group designations such as "the blind," "the
retarded" or "the disabled" are inappropriate because they do
not reflect the individuality, equality or dignity of people with disabilities.
Further, words like "normal person" imply that the person with a disability
is not normal, whereas "person without a disability" is descriptive
but not negative. Table 2 shows examples of positive and negative phrases.
Table 2: "AT A
GLANCE" GUIDE FOR USING PEOPLE FIRST LANGUAGE
|
People First Phrases
|
Negative Phrases
|
|
person with an intellectual, cognitive
or developmental disability
|
retarded; mentally defective
|
|
person who is blind or person who is
visually impaired
|
the blind
|
|
person with a disability
|
the disabled, handicapped
|
|
person who is deaf
|
hearing impaired; deaf and dumb
|
|
person who is hard of hearing
|
suffers a hearing loss, the deaf
|
|
person who has multiple sclerosis (MS)
|
afflicted by MS
|
|
person with cerebral palsy (CP)
|
CP victim
|
|
person with epilepsy, person with
seizure disorder
|
epileptic
|
|
person who uses a wheelchair
|
confined or restricted to a wheelchair
|
|
person who has muscular dystrophy (MD)
|
stricken by MD
|
|
person with a physical disability
|
crippled; lame; deformed
|
|
person without a disability
|
normal person (implies that the person with
a disability is not normal)
|
|
unable to speak, uses synthetic speech
|
dumb; mute
|
|
person with psychiatric disability or a
person with a mental illness
|
crazy; nuts
|
|
person who is successful, productive
|
has overcome his/her disability; is courageous
(when it implies the person has courage because of having a disability)
|
|
person with chronic pain disorder
|
pained person
|
This section outlines some etiquette
considerations to keep in mind while working with individuals with different
types of functional and/or access needs and disabilities.
Ask before you help
Just because someone has a disability,
don't assume he or she needs help. If the setting is accessible, people with
disabilities can usually get around fine. Adults with disabilities want to be
treated as independent people. Offer assistance only if the person appears to
need it. If the person does want help, ask how before you act.
Be sensitive about physical contact
Some people with disabilities depend on
their arms for balance. Grabbing them- even if your intention is to
assist-could knock them off balance. Avoid patting a person on the head or
touching his or her wheelchair, scooter or cane. People with disabilities
consider their equipment part of their personal space. Additionally sometimes
people with disabilities have a sensitivity to touch and touching them can put
them in a life threatening situation. When in doubt, ask how you can help.
Think before you speak
Always speak directly to the person with a
disability, not to his companion, aide or sign language interpreter. Making
small talk with a person who has a disability is simple; just talk to him as
you would with anyone else. Respect his privacy. If you ask about his disability,
he may feel like you are treating him as a disability, not as a human being;
however, many people with disabilities are comfortable with children's natural
curiosity and do not mind if a child asks them questions.
Don't make assumptions
People with disabilities are the best judge
of what they can or cannot do. Don't make decisions for them about
participating in any activity. Depending on the situation, it could be a
violation of the ADA to exclude people because of a presumption about their
limitations.
Respond graciously to requests
When people who have a disability ask for
an accommodation at the meeting location, it is not a complaint. It shows they
feel comfortable enough in your establishment to ask for what they need. If
they get a positive response, they will probably be more inclined to tell
others about your fairness and consideration in providing equal access to the
emergency planning process.
Evacuating and Transporting IFAN
Local planners should plan for individuals
who do not have transportation and those who may need accessible vehicles in
order to safely evacuate. To overcome these challenges, emergency planners
should work with local emergency preparedness partners to identify local
resources and existing transportation plans. These partners include city,
county, and state departments of transportation and transit agencies, who can
help to identify and transport residents in emergencies.
For example:
Evacuating and transporting vulnerable
older adults in emergencies can be challenging for emergency planners. A 2005
AARP survey found that:
·
15%
of adults aged 50 years or older would not be able to evacuate their homes
without help. Of this group:
o
50%
would need help from someone outside their household
o
25%
of adults aged 75 years or older would need help3
Older adults are also more likely to not
have access to a car, and many use medical equipment or assistive devices that
are hard to transport. Even older adults with cars may need more time to
prepare than younger adults because of difficulties driving in heavy traffic or
medical conditions that make it unsafe for them to sit in traffic for long
periods. Another challenge for emergency officials is that some people may not
want to evacuate. Reasons include a distrust of government, fear of not
returning home, previous experiences in shelters and concerns about pets.
Depending on the emergency, officials can
use different types of evacuation methods.
·
Multi-tiered
evacuations may be useful when officials know when a hazard (such as a hurricane)
is likely to occur. Under this strategy, older adults are encouraged to
evacuate before other groups to reduce stress and the amount of time spent in
traffic.
·
Publically
assisted evacuation plans identify ways to provide transportation to people who
cannot evacuate on their own (e.g., because they do not own a car or cannot
drive).
Registries can be used to identify older
adults who know in advance that they will need help.
3Identifying
Older Adults and Legal Options for Increasing Their Protection During
All-Hazards Emergencies: A Cross-Sector Guide for States and Communities
Atlanta: U.S. Department of Health and Human Services; 2012.
Sheltering in Place, Social Distancing and Other Forms of Isolation
A majority of older adults live in the
community rather than in institutional settings, and many are only able to live
independently with help from friends, family members, caregivers or in-home
services that provide meals, home-based health care, and help with chores and
personal care needs.
Some emergencies require isolation measures
such as sheltering in place or keeping a physical distance from other people
during a disease outbreak (called social distancing). Isolation from their
support network may make community-dwelling older adults more vulnerable during
an event or disaster, and these potential risks should be addressed in
preparedness plans (see Figure 4).
Figure 4: Planning Concerns for IFAN
Sheltering in Place, Social Distancing and Other Forms of Isolation
|
Emergency Action
|
Definition of
Action
|
Planning
Concerns
|
|
Sheltering in place
|
Occurs when people are warned to remain
indoors and to make a shelter out of the place where they are located. Sheltering
in place may be necessary during an event such as a chemical spill or
radiation emergency.
|
·
Promoting
personal preparedness.
·
Communicating
risk in accessible formats
·
Educating
the public about safety issues
|
|
Social distancing
|
Refers to infection control measures
that limit the spread of pandemic influenza or other infectious agents by
reducing the opportunity for people to come in contact with infected persons
|
·
Planning
for disruptions in access to routine medical care
·
Managing
obstacles for in- home service providers to make health visits, deliver meals
or perform other home-based services
·
Managing
limitations in the continuity of operations plans of home health care agencies
|
|
Isolation due to circumstances
|
Occurs when people are isolated at home
because of weather or other environmental events, such as an ice storm or flooding
that interrupt normal daily activities.
|
·
Planning
for disruptions in access to routine medical care
·
Managing
obstacles for in- home service providers to make health visits, deliver meals
or perform other home-based services
·
Managing
limitations in the continuity of operations plans of home health care agencies
|
Sources: CDC,
www.bt.cdc.gov/planning/shelteringfacts.asp and CDC, Social Distancing
Law Project materials, www.cdc.gov/phlp.
At the core of the many discussions around
emergency management planning for individuals with functional and/or access
needs and disabilities has been how people with functional needs are
accommodated in shelter environments. The main question has been "How do
you provide equal access to the services provided in a shelter that allows for
all residents to maintain a reasonable level of independence at the
shelter?" To answer this question and to effectively plan inclusively, it
is important to be aware of how shelter operations work within the State of
Georgia. This section will provide an overview of shelter operations within
Georgia.
Sheltering in Georgia includes mass care
and feeding support for individuals who must evacuate their homes due to a
disaster or incident. Shelters must meet the nationally accepted standards of
the American Red Cross and will ideally, remain open no longer than 30 days, at
which time other arrangements will be made for temporary housing in coordination
with local, regional, state and federal agencies.
While in a shelter, individuals can expect
basic short term accommodations. These may include snacks, beverages, cold
meals or sandwiches, hygiene kits and usually a cot and blanket. In emergency evacuation
shelters, cots may be in limited supply and be assigned to those with the most
urgent need, usually based on health conditions. If the need for longer term
sheltering is identified, additional resources and services will be provided.
These may include cots, blankets, hot meals, and additional assistance with
equipment for those with functional needs.
There is a process for opening and
supporting shelters on the local level, and each ESF 6 Partner Agency plays a
valuable role in opening shelters and ensuring that individuals with
disabilities and functional and access needs are reasonably accommodated during
their stay. Additional partner agencies provide support to shelter operations
and are identified in the State Mass Care Shelter Plan:
|
Agency
|
Role in Sheltering
|
|
American Red Cross (ARC):
|
·
The
ARC is the lead voluntary agency for sheltering in Georgia and works closely
local EMAs to provide shelters and disaster relief services to citizens
forced to leave their homes during a disaster.
·
ARC
provides daily meals and snacks, cots, blankets and comfort kits, limited
first aid, health services and mental health counseling.
·
ARC
coordinates with DHS, local DFCS, and GDPH (ESF 8) to provide support to
shelters when needed.
·
ARC
also provides access to the ARC Safe and Well website which can assist
families in locating relatives from whom they have been separated.
|
|
Local Emergency: Management Agencies
local (EMAs):
|
·
Local
EMAs coordinate disaster response within their community.
·
Assist
in identifying and establishing shelters for impacted populations in their
community and in support of statewide events.
·
Local
EMAs will conduct shelter operations according to their LEOPs. If necessary,
local EMAs will request additional support for shelters through GEMA.
|
|
Georgia Emergency Management Agency
(GEMA):
|
·
GEMA's
mission is to protect life and property and to prevent and/ or reduce the
negative impact of natural and man-made events in Georgia.
·
GEMA
provides support to shelters through logistics and coordination of volunteer
agencies.
·
GEMA
disseminates public information related to shelter locations and provides
preparedness information to the public.
|
|
Georgia Department of Human Services
(DHS):
|
·
DHS
is the lead state agency for sheltering in Georgia under the Governor's
Executive Order.
·
DHS
coordinates with the American Red Cross to assist local EMAs in providing
shelters throughout the state so citizens will have a safe haven from storms
and other dangers that require them to evacuate their homes and communities.
·
DHS
provides staffing and logistical support for shelters through the DFCS, the
DAS and through coordination with the GEMA, partner agencies and volunteer
organizations.
|
|
Georgia Department of Public Health
(GDPH):
|
·
The
GDPH coordinates and provides staffing support to ARC and DHS in shelters
based on available resources and other public health priorities.
·
GDPH
coordinates healthcare staff to shelters to assist with the assessment of
individuals with functional and access needs and coordinates healthcare
staff with expertise in basic first aid and health services to supplement
ARC health services staff after ARC has depleted its immediate nursing
resources.
·
GDPH
is responsible for identifying alternate facilities where individuals who
are not able to reside in a shelter may receive resources and services that
can better meet their needs.
·
GDPH
is responsible for obtaining MOUs with alternate facilities prior to a
disaster, if possible and should arrange for transportation of these
individuals from the shelter to the alternate facility.
·
Transportation
will be handled in coordination with GEMA and the ARC. GDPH also coordinates
with local jurisdictions to assist in locating appropriate accommodations
for individuals who must be cared for in a hospital setting requiring more
intense medical care.
|
|
Georgia Department of Behavioral Health
and Developmental Disabilities (DBHDD):
|
·
DBHDD
provides treatment and support services to people with mental illnesses and
addictive diseases and support to people with developmental disabilities.
·
DBHDD
supports DHS, ARC and GDPH in shelters by providing staff with expertise in
crisis counseling and mental health to assist with assessments of shelter
residents and the provision of services to those residents, shelter staff
and other responders and their families.
|
|
Georgia Department of Agriculture (GDA):
|
·
The
GDA provides support to shelter operations through the provision of pet
shelters, pet food and other necessary items for pets and service animals.
·
GDA
also identifies and coordinates the location of pet friendly shelters near
general shelters to allow evacuees to care for their pets during disasters.
·
GDA
also supports DHS and ARC in the provision of food and food services for
shelters when requested.
|
|
Friends of Disabled Children and Adults
(FODAC):
|
·
FODAC
provides home health (mobility and daily living) equipment to people of any
age or disability, temporary or permanent, for medically necessary and
medically helpful reasons.
·
When
called upon, FODAC can provide this equipment to shelters to support the
needs of individuals with functional and access needs in shelters or in
support of any mass care response.
|
|
Georgia Advocacy Office (GAO):
|
·
GAO
can provide information and referral, support and services to individuals
with disabilities, mental illness and the elderly in shelters if requested.
|
|
Georgia Organizations Active in Disasters
(GAVOAD):
|
·
GAVOAD
is a coordinated group of statewide volunteer organizations that provide
various services to individuals, families and local communities during
disasters.
·
GAVOAD
support is coordinated through GEMA by the Volunteer Agency Liaison or
directly through coordination with DHS. GAVOAD organizations can provide
many types of services to shelters and individuals within shelters.
·
Some
of these services include, but are not limited to, day care assistance and
feeding. GAVOAD can also assist with providing recovery services after a
disaster to help individuals regain their independence and return to or as
close to their pre-disaster standard of living.
|
The following is the American Red Cross's
protocol for opening a shelter in Georgia.
1. Communication
occurs between local EMA and Red Cross regarding need for shelter. Either Red Cross
or local EMA can initiate communication. Red Cross Disaster Services works
closely with all local governmental entities (i.e., Emergency Management
Officesincluding police/sheriff/fire departments, Health Departments, etc.) to
make informed decisions.
2.
Upon
knowledge of "individuals with immediate, emergency living needs caused by
any disaster situation" Red Cross disaster services activates and begins
immediate determination of the following:
The approximate
location/boundaries of the disaster damage
The approximate
numbers of families that are affected
The types of
emergency living needs
The likelihood of a
shelter being needed
3.
Once
the determination has been made that a Red Cross shelter should be opened, a
facility will be chosen based on type of disaster, location in relation to
families in need, size, length of time the shelter is anticipated to be necessary
and availability of the facility, among other considerations.
4.
Red
Cross will call the contact individual at the selected facility. An
"opening time" will be determined by mutual agreement of Red Cross
and the facility representative. Red Cross will then notify the shelter team
that the shelter will open.
5.
Shelter
Team is activated and plans for the following functions to be covered (in
approximate sequence):
Shelter Management
Registration
Feeding
Health Services
Logistics
Sleeping/Dorm
Management
Client Services
Staff
Recruitment/Placement
6.
Red
Cross activates shelter support and feeding support volunteers for ARC headquarters.
7.
Red
Cross communicates with the following:
Red Cross Disaster
Public Affairs for media contact
Government Liaison
for pertinent related disaster information
Other partners with
resources pertinent/applicable for response situation, i.e., Food Bank, SPCA,
communications personnel for ham radio, etc.
8. Red Cross maintains
regular communication throughout the shelter operation with EMA and partner
agencies.
Shelter Size and Layout Considerations
Estimating Shelter Capacity- The standards
used by the American Red Cross are:
20 square feet per
person should be available for short-term sheltering and up to 40 square feet
per person for sheltering longer than 72 hours.
Individuals with
functional and access needs i.e., who use wheelchairs, lift equipment, a
service animal and personal assistance services can require up to 100 square
feet.
Shelter Staffing Training Requirements
Each shelter operator is required to
complete ARC Shelter training to work as a shelter volunteer or as a shelter
supervisor. The basic shelter operations course for all staff is 8 hours.
Shelter Managers complete an additional one-day course.
Each of the two courses instructs
participants on shelter operations and expectations of all volunteers and
shelter supervisors. Shelter staff may all be Red Cross volunteers or may be
composed of a mixture of Red Cross volunteers and staff, volunteers from DFCS,
volunteers from other state agencies or partner organizations.
Shelter Functions
Local jurisdictions have the responsibility
for utilizing all area resources before requesting state assistance.
Jurisdictions can find potential shelter staffing in a variety of locations,
including:
Local Jurisdiction
Personnel
Voluntary Agencies
Service and Faith
Based Organizations
Community Emergency
Response Teams (CERT)
Students from Area
Universities (consider working with the university to develop a method for
students to obtain credits for working in a disaster shelter)
Private Industry
(local community businesses)
Local Nursing
Associations
Georgia Nurse Alert
System (GNAS)
SERVEGA for Medical
Reserve Corps and Other Volunteers
Private Industry
Medical staffing
agencies
Home health
agencies
Public Health
Department Staff
Only those positions which are necessary
for the operation should be filled. It may be appropriate to combine duties
under a specific position when possible. Staffing will depend on the scale and
duration of the incident/operation/shelter. The following are the key shelter
functions:
Shelter Management- Provide
administrative support and supervision for all functions in the shelter and
ensure that the occupants' needs are being met.
Registration- Ensure that all
shelter occupants are registered upon arrival. Maintain system for checking
occupants in and out when they leave for any period of time. Manage the system of
record keeping for shelter registrations.
Feeding- Supervise the food preparation and
service in shelter. Ensure that the needed supplies for the food service are
available. Keep accurate records of food and supplies received and expended.
Dormitory Management/Sleeping- Set up sleeping
areas. Ensure that residents have assigned areas for sleeping. If applicable,
coordinate placement of cots and blankets in area.
Disaster Health/Mental Services- Under the
direction of the DHS consultant at chapter disaster operations, ensure shelter
personnel's health and safety, monitor for disease prevention, provide first
aid as needed and maintain records of health services provided.
Client Services- Organize and
administer child care, recreation, transportation and other services as needed.
Staff Recruitment/Records- Recruit, place
and support staff assigned to the shelter. Provide opportunities to shelter
residents to serve as volunteers in the shelter. Maintain records of all
workers that assist with shelter operation (including name, address and phone
number).
Logistics- Provide support for the use of the
facility. Ensure the safety, security, and sanitation for the shelter. Procure,
store and distribute supplies and equipment at the shelter.
This section of the toolkit will discuss
shelter intake and placement. This Shelter Placement Guide is to assist
Shelter supervisors, American Red Cross Health Services, American Red Cross
Disaster Mental Health, and local Public Health representatives to decide
whether an individual should remain at a shelter or be placed in an alternate
facility that can better serve their needs.
Alternate facilities include, but are not
limited to, nursing homes, private care homes, independent living centers,
motels/hotels or another general shelter with appropriate resources to meet the
individual's needs. Appropriate alternate facilities, transport and transfer of
individuals moving to an alternate facility will be coordinated by local,
district and state public health, the lead agency for Emergency Support
Function (ESF 8) in conjunction with the American Red Cross, ESF 6 (Mass Care)
and local Emergency Management Agencies.
This information should be used in
conjunction with the assessments conducted upon the individual's entry into the
shelter. If an individual has an immediate medical need, staff should call
911/local emergency services access number for transport to a hospital. Staff
recommendations should be discussed with each individual and include
information on services immediately available at the shelter and those that
would be more readily available at an alternate facility. If an individual
chooses not to follow the recommendation of shelter staff, ARC Health Services/local
Public Health representatives may ask the individual to sign an informed
consent. Staff should ensure that the individual signing understands that they
have made the choice to remain at the shelter against the recommendation of trained
staff and that certain equipment and/or services may not be immediately available
at the shelter.
This tool was developed by the State FNSS
Working Group to provide overall guidance to local jurisdictions in support of
FNSS planning for general shelters.
It may be modified to reflect the specific
plans of each local jurisdiction for determining placement of individuals in
general shelters versus alternate facilities.
FIGURE 5: SHELTER PLACEMENT GUIDE
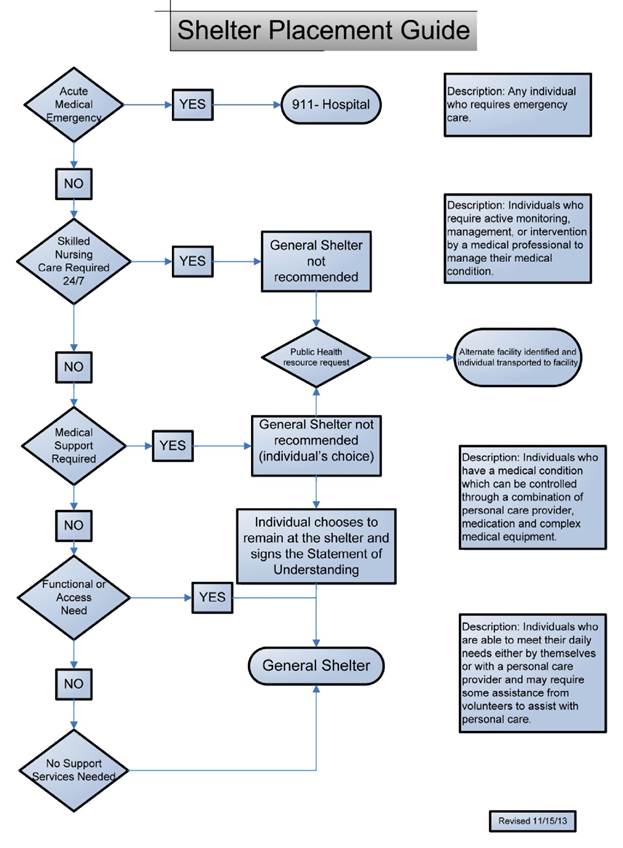
FIGURE 6: AMERICAN RED CROSS CMIST MODEL
WORKSHEET
CMIST Worksheet. Total number
of family included on this form_____.
DATE: _______. CLIENT/FAMILY NAME:_______. COUNTY/STATE:________.
Client location in shelter:_______. Interviewer:_________.
This is a document to cover possible considerations for
scenarios of access and functional needs. This is not an all- inclusive
checklist, but rather serves as a simple guideline for referral purposes.
COMMUNICATION
|
NEED:
|
ACTION:
|
|
□ Access to
auxiliary communication service
|
□ Provide written
materials in alternative format (Braille, large and high contrast print,
audio recording, or readers)
□ Provide visual
public announcements
□ Provide
qualified sign language or oral interpreter
□ Provide
qualified foreign language interpreter
|
|
□ Access to
auxiliary communication device
|
□ Provide access
to teletypewriter [TTY, TDD, or CapTel] or cell phone with texting
capabilities; pen and paper.
|
|
□ Replacement of
auxiliary communication equipment
|
□ Provide
replacement eyeglasses
□ Provide
replacement hearing aid and/or batteries
|
MAINTAINING HEALTH
|
NEED:
|
ACTION:
|
|
□ Special diet
□ Food Allergies
______ (type)
|
□ Provide
alternative (low sugar, low sodium, pureed, gluten-free, dairy- free,
peanut-free) food and beverages; ______ (diet type)
|
|
□
Medical
supplies and/or equipment for every day care (including medications) not
related to mobility
*For replacement eyeglasses or hearing aid, see
Communication
*For assistive mobility equipment (e.g., wheelchair),
see Independence
|
Refer to Disaster Health Services to
provide or procure one or more of the following:
□ Replacement
medication
□ Wound
management/dressing supplies
□ Diabetes
management supplies (e.g., test strips, lances, syringes)
□ Bowel or bladder
management supplies (e.g., colostomy supplies, catheters)
□ Oxygen supplies
and/or equipment
|
|
□ Assistance with
medical care normally provided in the home setting
□ Allergies
(environmental or other high risk) (type)
*For medical treatments that are not normally
provided in the home setting (e.g., dialysis), see Transportation
|
Refer to Disaster Health Services to
provide assistance with one or more of the following:
□ Administration
of medication
□ Storage of
medication (e.g., refrigeration)
□ Wound management
□ Bowel or bladder
management
□ Use of medical
equipment
□ Universal
precautions and infection prevention and control (e.g., disposal of
bio-hazard materials, such as needles in sharps containers)
|
|
□ Support for
pregnant women
□ Support for
nursing mothers;
□ Infant care
availability
|
□ Provide support
by ongoing observation
□ Provide support
and/or room for breastfeeding women
□ Assure diaper
changing area is available
|
|
□ Access to a
quiet area
|
□ Provide access
to a quiet room or space within the shelter (e.g., for elderly persons,
people with psychiatric disabilities, parents with very young children,
children and adults with autism)
|
|
□ Access to a
temperature-controlled area
|
□ Provide access
to an air-conditioned and/or heated environment (e.g., for those who cannot
regulate body temperature)
|
|
□ Mental health
care (e.g., anxiety and stress management)
|
□ Refer to
Disaster Mental Health Services
|
FIGURE 6: AMERICAN RED CROSS CMIST MODEL
WORKSHEET, continued
CMIST Worksheet. Total number
of family included on this form_____.
INDEPENDENCE
|
NEED:
|
ACTION:
|
|
□ Durable medical
equipment for individuals with conditions that affect mobility
|
□ Provide
assistive mobility equipment (e.g., wheelchair, walker, cane, crutches)
□ Provide assistive
equipment for bathing and/or toileting (e.g., raised toilet seat with grab
bars, handled shower, bath bench)
□ Provide
accessible cot (may be a crib, inclined head or other bed type)
|
|
□ Power source to
charge battery- powered assistive devices
|
□ Provide power
source to charge battery-powered assistive devices
|
|
□ Bariatric
accommodations
|
□ Provide
bariatric cot or bed
|
|
□ Service animal
accommodations
|
□ Provide area
where service animal can be housed, exercised, and toileted
□ Provide food and
supplies for service animal
|
|
□ Infant supplies
and/or equipment
|
□ Provide infant
supplies (e.g., formula, baby food, diapers, crib)
|
SERVICES, SUPPORT AND SELF-DETERMINATION
|
NEED:
|
ACTION:
|
|
□ Adult personal
assistance services
□ Child personal
assistance services
*IncI. general observation and/or assistance with non-medical
activities of daily living, such as grooming, eating, bathing, toileting,
dressing and undressing, walking, etc.
|
□ Identify family
member or friend caregiver
□ Assign qualified
shelter volunteer to provide personal assistance services
□ Contact local
agency to provide personal assistance services
□ Coordinate
childcare support such as play areas; age-appropriate activities; equal
access to resources.
|
TRANSPORTATION
|
NEED:
|
ACTION:
|
|
□ Transportation
to designated facility for medical care or treatment
□ Transportation
for non-medical appointment
|
□ Coordinate
provision of accessible shelter vehicle and driver for transportation
□ Contact local
transit service to provide accessible transportation
|
Actions:
□ No needs identified
□ Contact Shelter
Manager
□ Contact Disaster
Mental Health Services
□ Agency, please
provide agency name _____________.
□Other ___________.
Followup/Resolution/date ______________.
Disaster Health Services print
name/signature/date__________.
FIGURE 7: SAMPLE SHELTER PLACEMENT
RECOMMENDATION FORM & STATEMENT OF UNDERSTANDING
TO BE COMPLETED BY ARC HEALTH
SERVICES/PUBLIC HEALTH REPRESENTATIVE (Based on Information from the ARC
Initial Intake and Assessment Tool)
Name: _____ Age/DOB: _____
Tracking#: _____.
Does the individual
need immediate medical attention? Yes / No
Does the individual
have a medical condition that requires a nurse or doctor on a daily basis in
their home or at a medical office? Yes / No
If yes, recommend
alternate facility with medical support capability.
Does the individual
have a serious medical condition about which they are concerned? Yes /
No
If yes, refer to
Shelter Placement Guidance.
Does the shelter
have the ability to meet their needs? Yes/No
If no, recommend
alternate facility (could be another shelter with appropriate
support/resources).
Does the individual
appear to be appropriately alert and cognizant of the current situation? Yes/No
If no, refer to
Shelter Placement Guidance
Please indicate below any needs that cannot
be addressed at the shelter and any additional concerns based on the individual
assessment (provide detailed information on reasons for recommendation):
_________________________________________________________.
Recommended Shelter Type (circled): GENERAL ALT
FACILITY
Facility Name and Location (if known
orTBD): _____.
INDIVIDUAL STATEMENT OF UNDERSTANDING:
After being assessed by an ARC Health Services or public health representative
at the shelter, I acknowledge that I have been recommended for placement
in an alternate facility that can provide appropriate medical support to meet
my immediate or long-term medical needs. The reasons for the
recommendation were explained to me, and I have had the opportunity to ask
questions related to my placement. I understand that the purpose of the
alternate facility is to provide medical care and resources to individuals
whose medical needs exceed the level of care typically available in a General
Shelter. I understand that the services and medical care available at the
General Shelter may not meet my immediate or long term medical needs. However,
against the recommendation of a trained professional, I choose placement
in a General Shelter.
Print
Name: _____ Sign Name: _____
(Individual/Parent
or Guardian)
Date: _____. Phone: _____.
Alt Phone: _____.
ARC/Public Health Rep Name: _____. (Print)
Date: _____.
Title: _____
Signature: _____
Once the client intake and assessment have
been completed, shelter workers will have a clearer understanding of FNSS needs
of residents. The ARC has a process for requesting FNSS resources and services
through their existing chain of command. The shelter supervisor contacts ARC
Logistics and requests the needed equipment or service. The logistics manager
searches locally, if the ARC is not able to locate the equipment or service
locally, ARC Logistics searches regionally, then statewide, then nationally.
See Figure 14.0 for the resource request process outline.
FIGURE 8: ARC PROCESS FOR REQUESTING FNSS
RESOURCES
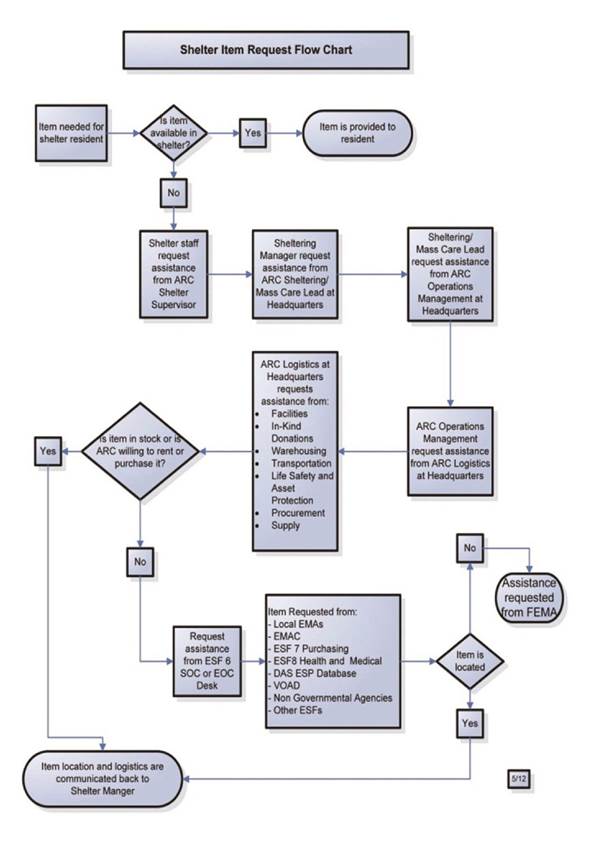
This section of the toolkit will:
Give a description
of the service type
Give examples of
the service type
Provide some
sources available locally, regionally, statewide and nationally
Key stakeholders from local agencies,
businesses, disability organizations, community-based organizations and
faith-based organizations that serve functional needs populations within the
jurisdiction should be identified and included in emergency planning committees.
The resources and capabilities of each entity should be assessed and integrated
into short and long-term plans in order to ensure that management of functional
needs starts at the local level before escalating to state and federal levels
of government.
Most cities and counties have local
resources for FNSS. It is recommended that local jurisdictions establish
working relationships and/or contingency contracts with local suppliers.
The support services include the following:
Reasonable
modification to policies, practices, and procedures
Durable medical
equipment
Consumable medical
supplies
Personal assistance
services
Other goods and
services as needed
Description: Resources and
services listed in this section address multiple types of functional needs
support services. In addition, many of the resources identified in this section
are available and accessible around the whole state.
Examples: Includes
different types of equipment to meet the various functional and access
needs-accessibility, mobility, communications support, toileting/bathing, feeding
support, bedding, dressing and additional medical supplies. Items A-K through
page 60 were developed by the Coalition or supplied by Coalition Members.
A. TIPS Guide for First Responders
This quick reference guide* provides
specific, practical tips for working with people who have a wide range of disabilities
including people with service animals, mobility challenges, cognitive
disabilities or mental illness, the blind or those with vision loss, and the
deaf or hard of hearing. The information is color-coded for easy access before,
during and after a crisis. The TIPS guide can be useful for anyone new to
working with individuals with functional and access needs.
* adapted from New Mexico's TIPS Guide

B. Establishment of Statewide Disability Network
Through an invitation letter from GEMA, the
Coalition invited organizations throughout Georgia that serve and advocate for
people with disabilities and older adults for the purpose of:
a)
enabling
those organizations to share Georgia's disaster preparedness and response
information with their constituencies; and
b)
to
ensure that state and local emergency planning incorporates the needs of
individuals with functional and access needs.
The community network currently consists of
52 stakeholder organizations around the state and continues to grow. Network
members receive information, tools and tips about emergency preparedness and
are invited to participate in Coalition sponsored Train-the-Trainer sessions
specifically geared towards assisting their clients and customers with their
emergency preparedness plans.

C. Emergency Preparedness Brochure
This brochure was created as a reference to
help individuals with disabilities and older adults prepare for emergencies.

D. Get Ready Tool Kit
The Get Ready Tool Kit consists of two
parts:
Part 1: Household Emergency Plan (The Plan)
Part 2: Emergency Plan Checklist (The
Checklist) The Plan is a form for individuals to record all the health information
for their household. When an emergency happens, all information needed is in
one place to grab and go. The checklist consists of two sections:
a)
Basic
Emergency Supplies
b)
Supplemental
Steps to an Effective Plan for individuals with functional and access needs.
The first section includes a list of items
to include in basic emergency kits and the second section identifies items to
enhance existing household emergency plans for individuals with functional and
access needs.

E. Train-The-Trainer Workshop
The Train-The-Trainer Workshop trains professionals,
family members and advocates working with individuals with functional and
access needs. The workshop trains the audience on presenting the Get Ready Tool
Kit and how to assist the audience to complete the tool kit. The course is FREE
of charge and participants will receive a certificate for their participation.
For information on scheduling a Train-The-Trainer Workshop for your community,
contact the State ADA Coordinator's office.

F. NOAA Weather Radio Special Needs Flyer
The Functional and Access Needs NOAA Weather
Radio Flyer was created to inform the public about the availability of the NOAA
Weather Radio adaptation accessories for purchase. Some of the accessories
include strobe lights, pillow vibrators, bed shakers and special text features
that are designed to notify individuals who are blind, deaf or hard- of-hearing
of severe weather alerts and warnings. These accessories will enable individuals
with functional and access needs to make informed decisions about their personal
preparedness.
G. Planning for Individuals who Use Assistive Technology (AT)
Individuals who use Assistive Technology
(AT) have unique emergency planning and response needs. This brochure was
created to provide information about Assistive Technology options and resources
within the State of Georgia. The brochure is intended for use by disability
service providers as well as individuals with functional and access needs to
assist them in better preparing for disaster or emergency situations.

H. Emergency Preparedness Fact Sheets
The Coalition has developed Fact Sheets
that focus on specific types of emergency and disaster situations that may
impact Georgians. Currently the developed Fact Sheets available are General
Preparedness, Earthquakes, Tornadoes, Hurricanes, Extreme Heat and Winter
Weather Advisories. The Fact Sheets are disseminated and posted monthly to
coincide with existing preparedness observances and disaster incidents and
events.

I. Communications Access Options for Individuals Who Are Deaf, Hard of
Hearing or Have Speech Difficulties Quick Reference Guide
This Guide was created to provide insight
to emergency managers, emergency planners, shelter supervisors, the local
public safety community, disability service providers and individuals with
disabilities about the various options available to provide accessible emergency
information to individuals who are deaf, hard of hearing or have speech
difficulties during emergency/disaster situations. The Guide has been developed
in a poster format and lists out multiple communication options, including
CapTel, Closed Captioning, Communication Boards, Pen/Pencil/Paper,
Pre-recorded, Messages/Information in ASL, Sign Language Interpreters, NOAA
Weather Radios with Accessories, TTY/TDD, Video Phone, Video Relay Service and
Video Remote Interpreting.

J. Coalition Information Fact Sheet
This Fact Sheet was created to provide
emergency managers, disability service providers and public health officials
information about the resources available through the Coalition. The Fact Sheet
is a one-page document that briefly summarizes the mission of the Coalition,
lists out the member agencies, list out the different sub-committees and gives
a brief explanation of the planning initiatives for the existing year.
All resources can be found within the
Appendix of this document. Additionally, Coalition materials are available for
free on the Georgia State ADA Coordinators website (http://ada.georgia.gov/emergency-preparedness).
Hard copies are also available by
contacting the Georgia State ADA Coordinator's office.

K. The Enhanced Services Program (ESP) Database
The Georgia Area Agencies on Aging maintain
an extensive database, ESP, of services of interest to seniors and people with
disabilities. The general public can access part of the online search tool at http://georgiaservicesforseniors.org.
This online search tool contains
information on some of Georgia's most requested services.
However, if someone needs more in-depth
information on these or other services they should contact their Area Agency on
Aging by calling 1-866-552-4464.
During a disaster or while recovery is
taking place, anyone needing resources for housing, durable medical equipment,
hospice or other topical information (examples are listed below), the ESP
database can be an important resource to access.

The following are primary categories of
information in the database:
Abuse/Neglect
Adult Day Care
Advocacy Assistance
Brain Injury/Spinal
Cord Injury
Care Management
Caregiver Services
Developmental
Disabilities
Emergency
Management Organizations
Emergency Response
Systems
End of Life
Planning
Financial
Assistance
Geriatric Assessment
Health Centers/Clinics
Health Conditions/Disease
Health Supportive
Products
Healthcare
Hospitals
Home Based Services
Home Care Providers
Home Health
Agencies
Hospice
Care/Palliative Care
Housing Options
Housing Services
Information/Referral
Insurance Programs
Legal Services
Leisure/Recreational
Medicaid Waiver/ Demonstration
Programs
Mental Health
Nursing Homes
Nutrition Services
Personal Care Homes
Prescription
Programs
Supportive Services
Transportation
Assistance
L. AAA Activities and Services
Aging Services Network
The Aging Services Network, created under
the authority of the Older Americans Act (OAA), is responsible for helping to
maintain the dignity and welfare of older adults. It is an essential partner in
preparedness planning for the vulnerable older population. The Aging Services
Network in Georgia is made up of the Georgia Department of Human Services,
Division of Aging Services, 12 Area Agencies on Aging (AAAs), numerous county
government agencies and small non-profit agencies that provide services (e.g.,
home health care or meal delivery) to older adults.
The AAA's One-Call "Gateway" to
Aging Services - 1-866-552-4464
Home Aid Solutions
(care coordination, meals, bathing, dressing, homemaking, etc.)
Disability Services
(ramps, rails, modification, assistive devices, education and more)
Caregiver Support
(individual guidance, support groups, training, respite, adult day care)
Wellness Programs
(senior fitness classes, training for organizers, medication education)
Georgia Cares
(prescription cost solutions, Medicare and health insurance education)
Ombudsman Program
(preserving residents' rights in long-term care facilities)
Elderly Legal
Assistance (individualized services for low-income seniors)
Elder Abuse
Prevention (public education about abuse, exploitation, neglect and fraud)
Civic Engagement
(through our volunteer recruitment program, gives individuals the opportunity
to donate their time to aiding seniors throughout the region)
Area Agency on Aging Contacts:
|
Northwest Area Agency on Aging
Counties: Bartow, Catoosa, Chattooga,
Dade, Fannin, Floyd, Gilmer, Gordon, Haralson, Murray, Paulding, Pickens,
Polk, Walker, and Whitfield
|
P.O.
Box 1798
Rome,
Georgia 30162-1798
1-800-759-2963
706-802-5506
Fax:
706-802-5508
Web:
www.nwgrc.org
|
|
Legacy Link Area Agency on Aging
Counties: Banks, Dawson, Forsyth,
Franklin, Habersham, Hall, Hart, Lumpkin, Rabun, Stephens, Towns, Union, and
White
|
Main
Office:
508
Oak Street, Suite 1 Gainesville, Georgia 30501 1-800-845-5465 770-538-2650 Fax:
770-538-2660 Web:
www.legacylink.org
|
|
Atlanta Regional Commission Area
Agency on Aging
Counties: Cherokee, Clayton, Cobb,
DeKalb, Douglas, Fayette, Fulton, Gwinnett, Henry and Rockdale
|
40
Courtland Street, NE Atlanta, Georgia 30303 1-800-676-2433 404-463-3333 Fax:
404-463-3264
Email: aginginfo@atlantaregional.com Web:
agewiseconnection.com
|
|
Southern Crescent Area Agency on
Aging
Counties: Butts, Carroll, Coweta, Heard,
Lamar, Meriwether, Pike, Spaulding, Troup and Upson
|
Main
Office:
13273
Highway 34 East Franklin, Georgia 30217 1-866-854-5652 706-407-0033
(Franklin area) 678-552-2838 (Atlanta area)
Fax:
770-854-5402 (Atlanta area) 706-675-9210 (Franklin area) Email: scaaa@scaaa.net Web:
www.scaaa.net
|
|
Northeast Area Agency on Aging
Counties: Barrow, Clarke, Elbert,
Greene, Jackson, Jasper, Madison, Morgan, Newton, Oconee, Oglethorpe and
Walton
|
305
Research Drive Athens, Georgia 30605 1-800-474-7540 706-369-5650 Fax:
706-425-3370 Web: www.negrc.org
|
|
River Valley Area Agency on Aging
Counties: Chattahoochee, Clay, Crisp,
Dooly, Harris, Macon, Marion, Muscogee, Quitman, Randolph, Schley, Stewart,
Sumter, Talbot, Taylor and Webster
|
Main
Office:
1428
Second Avenue
Columbus,
Georgia 31902
1-866-552-4464
Fax:
770-854-5402
Fax:
706-256-2940
Web: www.rivervalleyrcaaa.org
|
|
Middle Area Agency on Aging
Counties: Baldwin, Bibb, Crawford,
Houston, Jones, Monroe, Peach, Pulaski, Putnam, Twiggs and Wilkinson
|
175-C
Emery Highway
Macon,
Georgia 31217
1-888-548-1456
478-751-6466
Fax:
478-751-6517
Email: aging@mg-rc.org
Web: www.middlegeorgiarc.org/aaa.php
|
|
Central Savannah River Area
Agency on Aging
Counties: Burke, Columbia, Glascock,
Hancock, Jefferson, Jenkins, Lincoln, McDuffie, Richmond, Screven,
Taliaferro, Warren, Washington and Wilkes
|
3023
River Watch Parkway, Suite A
Augusta,
Georgia 30907
1-866-552-4464
706-210-2018
Fax:
706-210-2024
Web: www.csrarc.ga.gov
|
|
Heart Area Agency on Aging
Counties: Appling, Bleckley, Candler,
Dodge, Emanuel, Evans, Jeff Davis, Johnson, Laurens, Montgomery, Tattnall,
Telfair, Toombs, Treutlen, Wayne, Wheeler and Wilcox
|
331
West Parker Street Baxley, Georgia 31513 1-888-367-9913 912-367-3648 Fax:
912-367-3640 Web: www.hogarc.org
|
|
Southwest Area Agency on Aging
Counties: Baker, Calhoun, Colquitt,
Decatur, Dougherty, Early, Grady, Lee, Miller, Mitchell, Seminole, Terrell,
Thomas and Worth
|
1105
Palmyra Road Albany, Georgia 31701 1-800-282-6612 229-432-1124 Fax:
229-483-0995 Web:
www.sowegacoa.org
|
|
Southern Area Agency on Aging
Counties: Atkinson, Bacon, Ben Hill,
Berrien, Brantley, Brooks, Charlton, Clinch, Coffee, Cook, Echols, Irwin,
Lanier, Lowndes, Pierce, Tift, Turner and Ware
|
1725
South Georgia Parkway, West
Waycross,
Georgia 31503
1-888-732-4464
912-287-5888
Fax:
912-285-6126
Email:
wttaft@sgrc.us
Web:
www.sgrc.us
|
|
Coastal Area Agency on Aging
Counties: Bryan, Bulloch, Camden,
Chatham, Effingham, Glynn, Liberty, Long and McIntosh
|
127
F Street
Brunswick,
Georgia 31521 1-800-580-6860 Fax: 912-262-2313 Web: crc.ga.gov
|
|
|
|
M. GaMap2Care- Find Facility
Finding information about a specific
facility or facility type (nursing home, personal care home) in the state is a
simple matter of using our new GaMap2Care mapping application or our Find a
Facility search tool.
Please note: There is a new type
of licensed facility called "Assisted Living Community" that has not
yet been included in these search tools. Assisted Living Communities are
Personal Care Homes that serve 25 or more residents, employ certified
medication aides and have opted to become licensed as Assisted Living Communities.
To see a list of currently licensed Assisted Living Communities visit: http://dch.georgia.gov/gamap2care-find-facility
N. Centers for Independent Living
Centers for Independent Living are
non-residential, community-based organizations, governed and staffed by people
with disabilities that offer a wide variety of services to consumers with
disabilities and their families. The foundation of these services is the
peer-to-peer relationship, where people with disabilities act as mentors for
other people with disabilities, showing them by example how to help themselves
and to live independently. The core services that CILs provide are:
Individual Advocacy
and Systems Advocacy
Peer Counseling
Information and
Referral
Independent Living
Skills Training
Depending on the needs of the communities
they serve, CILs may provide other services that vary from one center to
another. Contact information for the CILs located within the state:
|
No.
|
Organization Name
|
Website
|
Address
|
City
|
Zip Code
|
Phone
|
|
1
|
Access Center for Independent Living
|
http://www.access4il.org
|
430 Prior Street, Suite 120
|
Gainesville
|
30501
|
770-534-6656
|
|
2
|
Bain Center for Independent Living
|
http://www.baincil.org
|
314 Shotwell Street
|
Bainbridge
|
39818
|
229-246-0150
|
|
3
|
Disability Connections
|
http://www.disabilityconnections.com
|
170 College Street
|
Macon
|
31201
|
478-741-1425
|
|
4
|
Disability Link
|
http://www.disabilitylink.org
|
755 Commerce Drive, Suite 105
|
Decatur
|
30030
|
404-687-8890
|
|
5
|
Disability Link- Northwest
|
|
411 Broad Street
|
Rome
|
30161
|
706-314-0008
|
|
6
|
Living Independence for Everyone, Inc.
(LIFE)
|
http://www.liefcil.com
|
12020 Abercom Street
|
Savannah
|
31419
|
800-948-4824
|
|
7
|
Middle Georgia CIL, Inc.
|
|
170 College Street
|
Macon
|
31201
|
478-741-1425
|
|
8
|
Multiple Choices Center for Independent Living
|
http://www.multiplechoices.
us/mcilgraphics.aspx
|
850 Gaines School Road
|
Athens
|
30605
|
706-549-1020
|
|
9
|
Statewide Independent Living Council of
Georgia
|
www.silcga.org
|
755 Commerce Drive Suite 145
|
Decatur
|
30030
|
770-270-6860
|
|
10
|
Walton Options for Independent Living
Inc.
|
http://www.waltonoptions.org
|
PO Box 519 948 Walton Way
|
Augusta
|
30903
|
706-724-6262
|
O. ADA Guide for Local Government Emergency Preparedness
This website is sponsored by the Department
of Justice. One of the most important roles of local government is to protect
its citizens from harm, including helping people prepare for and respond to
emergencies. Making local government emergency preparedness and response
programs accessible to people with disabilities is a critical part of this
responsibility. Having these programs accessible is also required by the
Americans with Disabilities Act of 1990 (http://www.ada.gov/emergencyprepguide.htm).
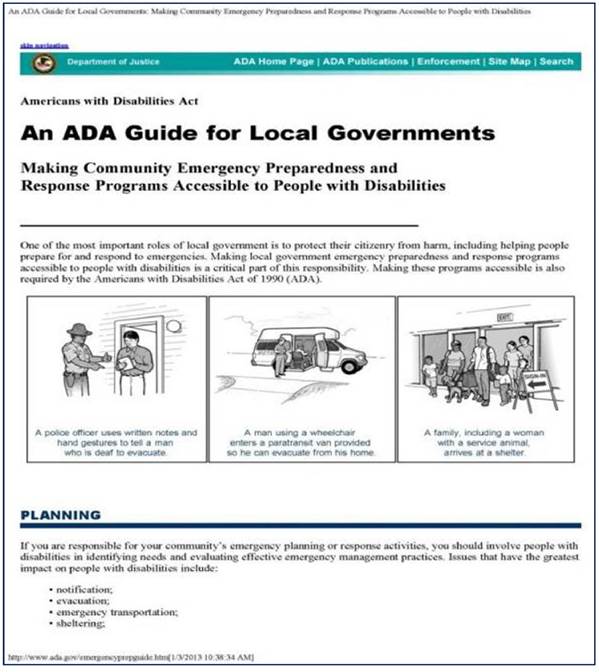
Despite best efforts and advance planning,
some persons will arrive at the shelter without durable medical equipment
(DME).
Description: Durable
medical equipment is any medical equipment used in the home to aid in a
better quality of living. It is medical equipment used by persons with a disability
to maintain their usual level of independence. Note: A person who uses durable
medical equipment may or may not have a medical need.
DME meets these criteria:
Durable
(long-lasting)
Used for a medical
reason
Not usually useful
to someone who isn't sick or injured
Used in your home
Examples: DME includes
Air-fluidized beds
Blood sugar
monitors
Canes (however,
white canes for the blind aren't covered)
Commode chairs
Continuous Positive
Airway Pressure (CPAP) machine
Crutches
Home oxygen
equipment and supplies
Hospital beds
Infusion pumps (and
some medicines used in infusion pumps if considered reasonable and necessary)
Nebulizers (and
some medicines used in nebulizers if considered reasonable and necessary)
Patient lifts (to
lift patients from bed or wheelchair by hydraulic operation)
Suction pumps
Traction equipment
Walkers
Wheelchairs
Nebulizers
Transfer boards
Accessible and/or
bariatric cots
Privacy screens
Resources for Durable Medical Equipment
One of the primary sources for the
acquisition of durable medical equipment (DME) is Tools for Life. Tools for
Life, Georgia's Assistive Technology Act Program, is dedicated to increasing
access to and acquisition of assistive technology (AT) devices and services for
Georgians of all ages and disabilities so they can live, learn, work and play
independently and with greater freedom in communities of their choice.
Other Sources for Obtaining Reused/Gently Used DME/AT Devices:
The Georgia AT Depot
Georgia AT Depot is a state-wide buying Cooperative
for Assistive Technology for customers in the State of Georgia. The Georgia AT
Depot is modeled after the Maryland AT Co-op, which has operated a successful
cooperative buying program since 1998 (http://www.atdepot.org/).

gTRADE
gTrade is Georgia's Online Equipment
Exchange, encourages members to offer AT and DME for sale or donation to others
who may benefit from using technology unneeded by others (http://www.gtradeonline.org/).

FODAC
Friends of Disabled Adults and Children
(FODAC) is Georgia's statewide provider of home health equipment and durable
medical equipment. FODAC has distributed 20,000 wheelchairs and thousands of
other pieces of DME since 1986. Internationally, 65 countries have received
some equipment over those years (www.fodac.org).
FODAC has indicated that they are willing
to partner directly with local jurisdictions to supply DME to support disaster
survivors in their communities.

The Dollars and Sense Funding Guide
The Dollars and Sense Funding Guide is an online
database with possible funding sources and strategies to obtain funding for
assistive technology (http://web-helps.net/DS
Search/).

If local resources are not available for
DME equipment then the following may be available:
GEMA Shelter Trailers
In 2012, GEMA purchased the top five pieces
of Durable Medical Equipment typically requested in American Red Cross Shelters
around the country. This included wheelchairs, walkers, transfer boards,
walking canes, raised toilet seats and privacy screens. The equipment is stored
in shelter trailers across the state in the communities that are most likely to
host evacuees during a disaster incident and can be accessed upon request.
GEMA Warehouse Durable Medical Equipment
In 2013, GEMA worked with state approved
medical equipment vendors to purchase Durable Medical Equipment that could be
stored and accessed for delivery to shelters. GEMA collaborated with FODAC to
receive, palletize and store the equipment in the organization's Stone Mountain
warehouse to ensure that the equipment could be accessed and transported to
support local disaster response operations upon request.
Figure 16.0 depicts the process for
requesting durable medical equipment/ consumable medical supply resources
through the State Operations Center, ESF #6. This equipment and supplies are
intended to be activated in a major or catastrophic event impacting Georgia. Local
partners should pre-identify locations within their communities, counties and
regions that can meet these needs and exhaust all possibilities before
requesting this state cache of equipment.
FEMA Process for Requesting Durable Medical Equipment Cache
In 2012 FEMA entered into contract with
various durable medical equipment providers around the country. DME can be
requested from FEMA through the State of Georgia to assist with disaster
response and recovery effort. The request must be made through the state
and a Presidential Disaster Declaration is required for request.
FIGURE 9: DURABLE MEDICAL EQUIPMENT
REQUESTS THROUGH THE STATE
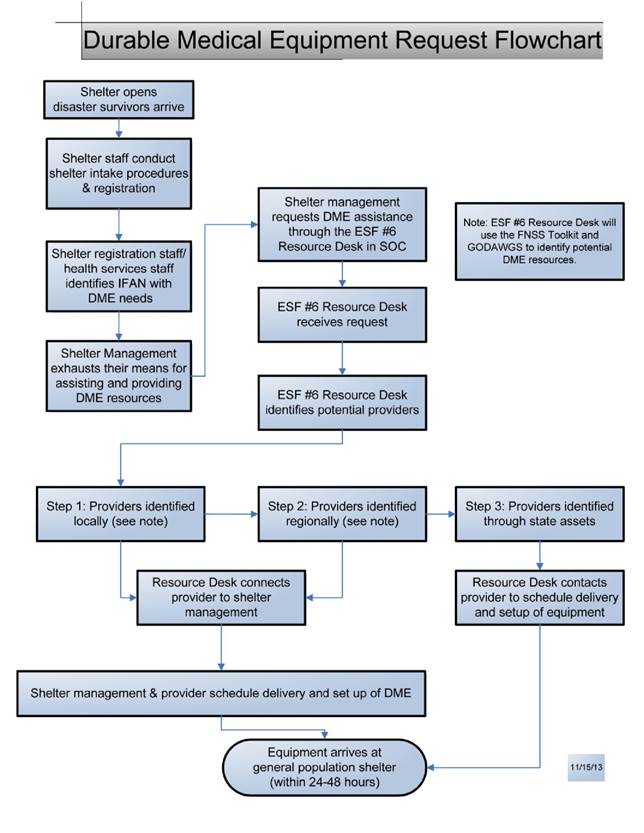
Description: Consumable
Medical Supplies (CMS) are those non-durable supplies and items that enable
recipients to increase their ability to perform activities of daily living.
Consumable Medical Supplies are of limited usage and must be replaced on a
frequent basis.
Consumable Medical Supplies are non-durable
medical supplies that:
Are usually disposable
in nature
Cannot withstand
repeated use by more than one individual
Are primarily and
customarily used to serve a medical purpose
Generally are not
useful to a person in the absence of illness or injury
May be ordered
and/or prescribed by a physician
Examples:
Adult disposable
briefs
Catheters
Wipes
Disposable gloves
Surgical masks
Disposable or
washable bed, or chair pads and adult sized bibs
Ensure or other
food supplements
Feeding tubes and
supplies
Dressings
Hearing aid
batteries, cords and routine maintenance and cleaning
CMS Resources:
Consumable Medical Supplies will be
available at local pharmacies, durable medical equipment suppliers or local
stores (i.e., Target and Wal-Mart).
If local resources are not available for
DME equipment then the following may be available:
GEMA Shelter Trailers: Between 2009-
2010, GEMA partnered with local EMA's to identify host shelter communities. The
communities that agreed to host shelters were awarded shelter supply trailers.
Each trailer around the state contains Consumable Medical Supplies required to
operate shelters. Supplies include (but are not limited to) briefs, bandages,
disposable patient care gloves, cotton supplies, cold packs, hot packs,
thermometers, alcohol, stethoscopes, wet wipes, baby bottles, oral syringes and
CPR Pocket masks.
During a disaster event, people will arrive
at shelters without their pharmaceutical medicines. In order to maintain
independence and reduce medical crisis events, these medicines will need to be
replaced as soon as possible.
Description: A pharmaceutical
drug also referred to as a medicine or (loosely) medication, can be roughly
defined as any chemical substance intended for use in the medical diagnosis,
cure, treatment or prevention of disease.
American Red Cross Pharmacy Support
The Red Cross has the ability to offer
shelter resident replacement medications during their stay. The procedure for
replacing essential prescription medications for shelter residents includes the
following:
Red Cross will
contact the pharmacy where the resident has been getting their medication. If
it is inaccessible or too far away, they will have the prescription transferred
to a pharmacy nearer the shelter. Verify first that the prescription is
current, and when the last refill was obtained to be sure the resident had the
medication and was taking it regularly. Check all current prescriptions on file
to be sure all needed prescriptions are replaced.
If there is
insurance coverage, determine if the refill is eligible for coverage. Pharmacists
may have the ability to get insurance companies to pay for emergency refills
due to disasters. Pharmacists have the knowledge and ability to access
appropriate authorities for authorization of emergency refills for Medicaid covered
residents.
Prescriptions from
large chain pharmacies are generally available at any store within their chain
through computerized records.
If there are no
refills available on a resident's prescription, ARC Health Services will
contact their health provider (or clinic) for a new prescription and have it
called in to a designated pharmacy nearby.
If the resident
does not know what medications they were taking, ARC Health Services will
contact their health provider (or clinic) for a list of medications, get
prescriptions and have it called in to a designated pharmacy nearby.
If the resident's
pharmacy and usual health care provider cannot be reached, ARC Health Services
can arrange for them to be seen at the nearest urgent care center, clinic or
emergency room where they can be evaluated and receive new prescriptions. ARC
Health Services will negotiate the lowest possible rate and will open a case
for the resident so a debit card can be issued to cover the expense.
The Shelter Supply
Officer will pick up the prescription(s) and pay for them with a Red Cross
purchase card.
Sometimes the
resident has insurance coverage or personal means to pay for their medication
and will only need assistance with making logistical arrangements to obtain
their medication.
If Red Cross does
provide medications to a resident, generally only a 1-2 week supply is
purchased for the time the resident is expected to be in the shelter. Once the
resident leaves the shelter, case workers and ARC Health Services will evaluate
the resident's ongoing needs and may authorize up to a month's refill on all
medications, including those refilled while the resident stayed in the shelter.
Note to Planners: Public Health
personnel may be requested to fill the role of the ARC Health Services representative
and should be aware of the Red Cross procedures for medications in shelters. In
addition, Public Health may be requested to assist with obtaining and/or
coordinating medications and other resources for shelters.
Department of Public Health, Pharmacy
Section
The mission of the Pharmacy Section of the
Department of Public Health is to provide current drug and disease information
and/or coordinate the acquisition of high quality, cost-effective
pharmaceuticals to health professionals working within the public health
system, for use in disease prevention and the promotion of the health and
well-being of Georgians.
The Pharmacy Director plans, organizes, and
directs the pharmacy service programs of the Department of Public Health by
coordinating the activities of pharmacists, other division and district health
professionals and administrative and technical personnel involved in the
statewide delivery of drugs and vaccines to public health clinics.
Pharmaceuticals are ordered and distributed
through District Drug Coordinators from pharmacy manufacturers, pharmacy
wholesalers, the Division or TB pharmacy, or other contracted organizations. (http://health.state.ga.us/programs/pharmacy/)
Description: Personal
Assistance Services (PAS) formal and informal services provided by a person
that enable children and adults to maintain their usual level of independence.
A Personal Assistant (PA) could be a family member, friend or professional.
Other names for this person are attendant or caregiver.
Examples:
Assist persons in
maintaining their usual level of independence activities of daily living such
as grooming, eating, bathing, toileting, dressing and undressing, walking/transferring,
maintaining health and safety, taking medications, communicating, and accessing
programs and services.
Provide support to
persons with intellectual, cognitive and mental health conditions
Provide
interpreters and/or other communication support to assist persons who require
communication assistance deaf or hard of hearing and blind or low vision,
speech disabilities, language/cultural differences
Provide assistance
to individuals who have conditions that affect mobility
Provide assistance
to children and adults with chronic but stable respiratory conditions (heart
disease, asthma, emphysema, allergies, etc.)
Provide assistance
to children and adults with temporary limitations (post-surgery, injuries,
pregnancy, etc.)
Provide assistance
to children and adults who require dialysis
PAS Resources:
Center for Personal Assistance Services:
The PAS
Center provides research, training,
dissemination and technical assistance on issues of personal assistance services
(PAS) in the United States. The services and information accessed through the
PAS Center website can be utilized to provide FNSS Services to individuals during
disaster and emergency incidents.
(http://www.pascenter.org/state_based_stats/index.php?state=georgia)

The following are some examples of
Promising Practices in PAS:
Caretracker - IHSS Public Authority in
Santa Barbara County, CA (http://www.pascenter.org/emergency/Caretracker_Promising_Practice.php)
Shelter Volunteer Caregiver Training
Emergency Management Disability and Aging Coalition (EMDAC) in Louisiana
(http://www.pascenter.org/emergency/Shelter_Volunteer_Promising_Practice.php)
Using Medical Reserve Corps for PAS in
shelters -Missouri State Emergency Management Agency
(http://www.pascenter.org/emergency/Reserve_Corps_Promising_Practice.php)
State Personal Care Programs- States have the
option of offering personal care services (PCS) as a Medicaid benefit. States
have considerable discretion in defining PCS but programs typically involve
non-medical assistance with activities of daily living (e.g., bathing and
eating) for participants with disabilities and chronic conditions. Unlike
waivers, the PCS benefit must be available to all categorically eligible groups
but states can opt to include the medically needy (those who spend down to the
state standard because of medical expenses).
(http://www.pascenter.org/statehttp://www.pascenter.org/state_based_stats/PAS_contact_info.php?state=georgia&title=Contact+Info+for+Medicaid+PAS)
FEMA's MOU with National Personal Assistant
Service Company:
The Robert T. Stafford Disaster Relief and Emergency Assistance Act (Public Law
93-288), as amended after the hurricane season of 2005, assigned new
authorities to FEMA, including the provision of services to individuals with
functional and access support needs in congregate facilities. FEMA awarded the
PAS contract to augment the ability of states, tribes and territories to help
individuals with functional and access needs maintain their health, safety and
independence in congregate facilities after a Presidential declaration. FEMA
has contracts with two personal assistance services providers. The PAS contract
provides two levels of support to help individuals with functional and access
needs maintain their independence in congregate facilities, including:
Basic personal
care, such as grooming, eating, bathing, toileting, dressing and undressing,
walking, transferring, and maintaining health and safety.
Higher level of
care, including changing dressings on wounds (such as pressure point sores),
administering medications / injections (such as insulin), catheterization, and
respiratory care (to include mechanical ventilation) when allowed by the state
or territory.
A maximum of 50 PAS staff per contractor
will deploy a minimum of 24 hours after the task order has been issued and
funding has been secured. Eligible applicants are state, tribal, or territorial
governments that request FEMA to provide PAS in congregate facilities after a
Presidential declaration.
The purpose of this section is to provide
local jurisdictions with recommendations for meeting the various needs
(including, but not limited to, assistive technology and communication needs)
of displaced populations with functional and access needs in a
disaster/emergency.
Description: Individuals with
or without disabilities who have access or functional needs should be given the
same information provided to the general population using methods that are
understandable and timely. Planning for effective communication requires
pre-emergency planning for auxiliary aids and services to meet the
communication needs of all shelter residents.
Examples:
Hearing Aids
TTY/TDD Phones
CapTel Phones (for
captioned telephone)
Computer Access
Realtime Translation (CART)
Hearing Aid
Batteries (different sizes including batteries for cochlear implants)
Synthesizers (used
with PCs for text-to-speech)
Screen Readers
Screen
Magnification Programs
Scanning Systems
for Low Vision Users
Videophone
Video Remote
Interpreter
Pencil and Paper
GACHI, Serving the Deaf & Hard of
Hearing:
Established in 1989, GACHI is a statewide nonprofit organization that provides
a variety of assistive services to the deaf and hard of hearing, their family
members, friends, and local state and federal agencies. In addition to the main
office in Decatur, GACHI operates satellite offices in Columbus, Cedartown,
Augusta, Macon and Hinesville. Services offered include:
Advocacy, including
educating others about ADA, encouraging customers to foster self-determination
as well as empowerment and independence
Information and
Referral
locating resources and referrals geared toward individuals with hearing loss
and speech issues and the people surrounding them
Community Education
& Outreach
educating others primarily through workshops and special event as well as
outreaching letting others know about GACHI, The Georgia Telecommunications
Equipment Distribution Program, offering free telecommunication devices to
qualified applicants (http://gachi.org/GATEDP)
Communications Access Options for
Individuals Who Are Deaf, Hard of Hearing or Have Speech Difficulties: This Guide was
created to provide insight to emergency managers, emergency planners, shelter
supervisors, the local public safety community, disability service providers
and individuals with disabilities about the various options available to
provide accessible emergency information to individuals who are deaf, hard of
hearing or have speech difficulties during emergency/disaster situations.
The Guide has been developed in a poster
format and lists out multiple communication options, including: CapTel, Closed
Captioning, Communication Boards, Pen/Pencil/Paper, Pre-recorded
Messages/Information in ASL, Sign Language Interpreters, NOAA Weather Radios
with Accessories, TTY/TDD, VideoPhone (vp), Video Relay Service (VRS) and Video
Remote Interpreting (VRI). The Guide is housed on the ADA Coordinators website.
(http://ada.georgia.gov)
General Effective Communication
Requirements under Title II of the ADA:
Provides tools and requirements for
communicating with all audiences including those with disabilities. (http://www.ada.gov/pcatoolkit/ch3 toolkit.pdf)
Georgia Registry of Interpreters for the
Deaf website: www.garid.org
This booklet is available for order at http://www.dawnsign.com/100-signs-for-emergencies.
List of Appendices
1) Georgia Emergency
Preparedness Coalition for Individuals with Disabilities & Older Adults
Agency Members Contact Information
2) Georgia
Stakeholders: Maps
Georgia Public
Health Districts Map
Georgia Department
of Human Services, Division of Family and Children Services Regional Map
American Red Cross
of Georgia Chapters Map
Medical Reserve
Corp Units of Georgia Regional Map
Georgia Department
of Behavioral Health and Developmental Disabilities Regional Map
GACHI, Serving the
Deaf and Hard of Hearing Regional Offices Map
DHS, Division of
Aging Services Planning and Service Areas Map, Area Agencies on Aging Regions
Georgia Independent
Living Center Regions Map
Georgia Regional
Commissions Map
GEMA Field
Coordinator Areas
3) Community Living
Options Post Disaster
Atlanta
Area School for the Deaf
Phone:
(404) 296-7101 VP: (404) 537-1222
Website:
www.aasdweb.com
American
Red Cross of Georgia
Phone:
1(866) RC-HELPS (1-866-724-3577) to reach your local chapter
Website:
www.redcross.org
Center
for Advanced Communications Policy-Georgia Institute of Technology
Phone:
(404) 385-4614
Website: www.cacp.gatech.edu/
Department
of Human Services, Division of Aging Services
Phone:
1(866) 55-AGING (552-4464)
Website: http://aging.dhr.georgia.gov
Department
of Human Services, Office of Facilities and Support Services
Phone:
(404) 651-6316
Website:
http://dhs.georgia.gov/office-facilities-support-services
DeKalb
County Emergency Management Agency
Phone:
(770) 270-0413
Website:
http://web.co.dekalb.ga.us/DK_Police/pol-dema.html
Federal
Emergency Management Agency
Phone:
(770) 220-5200
Website:
www.fema.gov
Friends
of Disabled Adults and Children
Phone:
(770) 491-9014 or 1-866-977-1204
Website:
www.fodac.org
Georgia
Advocacy Office
Phone:
(404) 885-1234 or Voice or TDD: 1(800) 537-2329
Website:
www.thegao.org
GACHI-
Serving the Deaf and Hard of Hearing
Video
Phone: 404-492-8472 Voice/TTY: (404) 292-5312 Voice/TTY Toll Free: (800)
541-0710 Fax: (404) 299-3642
Website:
www.gachi.org
Georgia
Department of Behavioral Health and Developmental Disabilities
Phone:
(404) 657-2258
Website: www.dbhdd.georgia.gov
Georgia
Department of Public Health, Division of Health Prevention, Emergency Preparedness
and Response
Phone:
(404) 657-2700
Website: www.health.state.ga.us
Georgia
Emergency Management Agency
Phone:
(404) 635-7000 or 1(800) TRY-GEMA (in Georgia only)
Website:
www.gema.ga.gov/
www.ready.ga.gov
Georgia
Radio Reading Service
Phone:
(404) 685-2820, Toll Free (800) 672-6173
Website:
www.garrs.net
Georgia
State Finance and Investment Commission-State ADA Coordinator's Office
Phone:
(404) 657-7313 TTY: (404) 657-9993
Website: www.ada.georgia.gov
Gwinnett
County Emergency Preparedness Coalition
Phone:
(770) 995-3339
www.gwinnettcoalition.org
www.gwinnetthelpline.org
Gwinnett,
Newton, Rockdale County Health Departments
Phone:
(770) 339-4260
Website: www.gnrhealth.com
Portlight
Strategies, Inc.
Phone
(Voice/TTY), (770) 330-5653 or (843) 817-2651
Website: www.portlight.org
The
Shepherd Center
Phone
(Voice/TTY) (404) 352-2020
Website:
www.shepherd.org
Southeast
ADA Center
Toll
Free Phone (Voice/TTY): (800) 949-4232 Phone (Voice/TTY) (404) 541-9001
Website: www.adasoutheast.org
Tools
For Life-The Alternative Media Access Network, Georgia Institute of Technology Enterprise
Innovation Institute
Phone:
(404) 894-0541 Toll Free: (800) 497-8665
The following are several Georgia maps of
potential stakeholders broken down by service delivery region or area around
the state. Each agency, association and organization has different designated
regions within the state. When planning, you will need to identify the specific
district, chapter or region for your locality. Please note that this is not a
complete set of maps of all potential stakeholders.
A. Georgia Public
Health Districts Map
B. Georgia Department
of Human Services, Division of Family and Children Services Regional Map
C. American Red Cross
of Georgia Chapters Map
D. Medical Reserve
Corp Units of Georgia Regional Map
E. Georgia Department
of Behavioral Health and Developmental Disabilities Regional Map
F. GACHI, Serving the
Deaf and Hard of Hearing Regional Offices Map
G. DHS, Division of
Aging Services Planning and Service Areas Map, Area Agencies on Aging Regions
H. Georgia Independent
Living Center Regions Map
I. Georgia Regional
Commissions Map
J. GEMA Field
Coordinator Areas
A. GEORGIA DEPARTMENT OF PUBLIC HEALTH (www.health.ga.us)
GEORGIA Public Health Districts
1-1 Northwest (Rome)
1-2 North Georgia (Dalton)
2 North (Gainesville)
3-1 Cobb-Douglas
3-2 Fulton
3-3 Clayton (Jonesboro)
3-4 East Metro (Lawrenceville)
3-5 DeKalb
4 LaGrange
5-1 South Central (Dublin)
5-2 North Central (Macon)
6 East Central (Augusta)
7 West Central (Columbus)
8-1 South (Valdosta)
8-2 Southwest (Albany)
9-1 Coastal (Savannah)
9-2 Southeast (Waycross)
10 Northeast (Athens)
B. GEORGIA DEPARTMENT OF HUMAN SERVICE, DIVISION OF FAMILY AND CHILDREN
SERVICES (dfcs.dhs.georgia.gov)
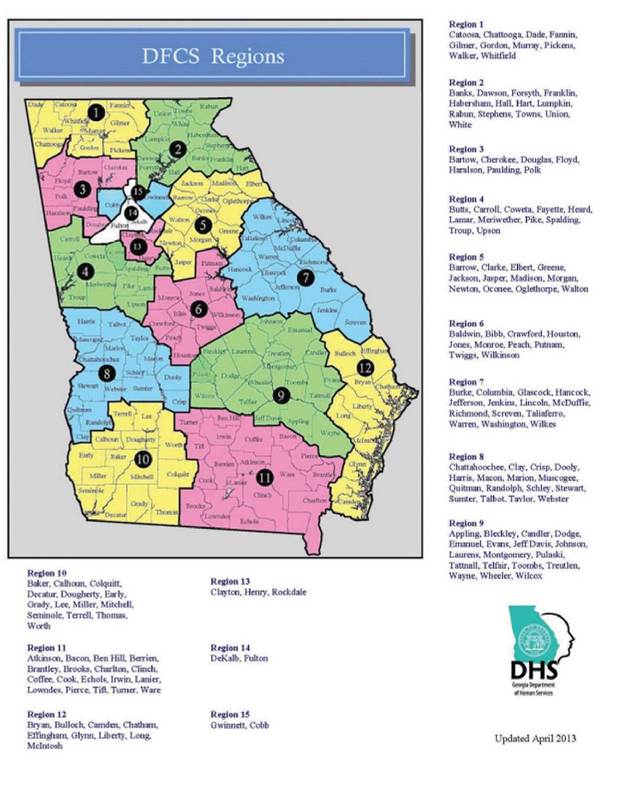

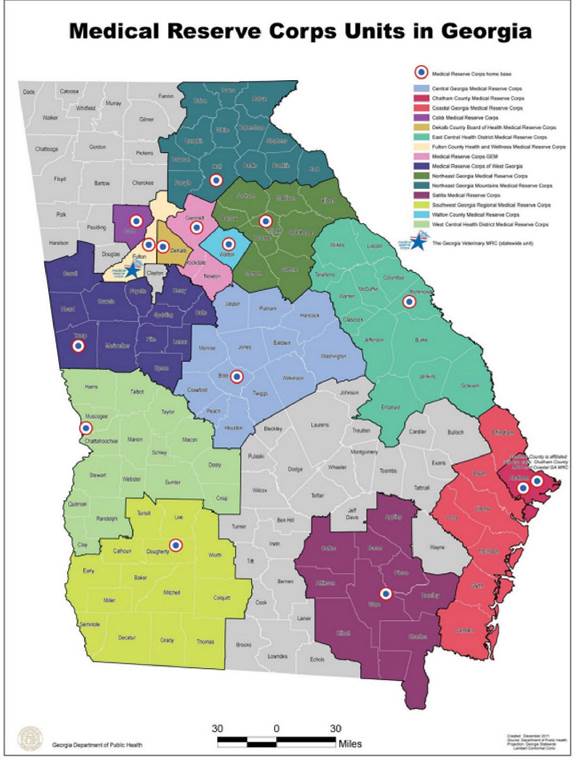
E. GEORGIA DEPARTMENT OF BEHAVIORAL HEALTH AND DEVELOPMENTAL DISABILITIES (www.dbhdd.georqia.gov)
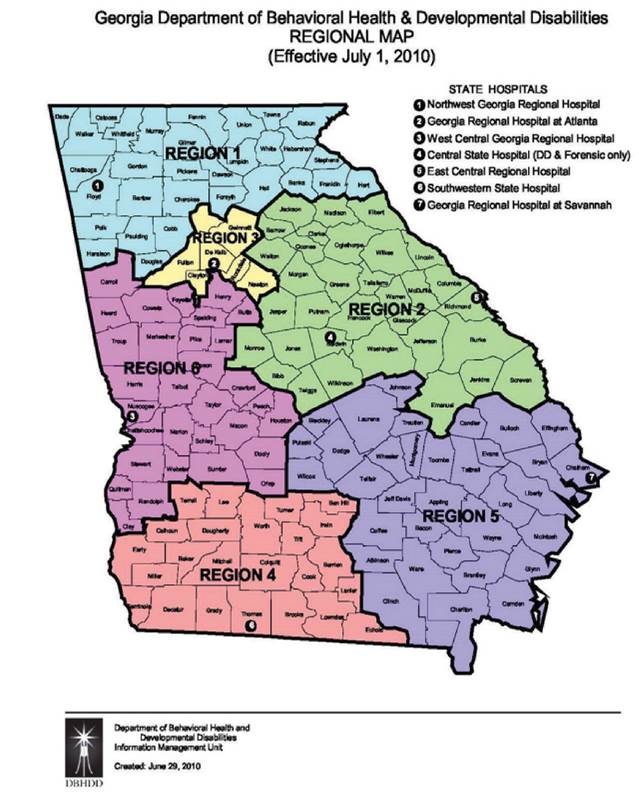
F. GACHI, SERVING THE DEAF & HARD OF HEARING (www.gachi.org)

G. DEPARTMENT OF HUMAN SERVICES, DIVISION OF AGING SERVICES, AREA AGENCIES
ON AGING (http://aging.dhs.georgia.gov)

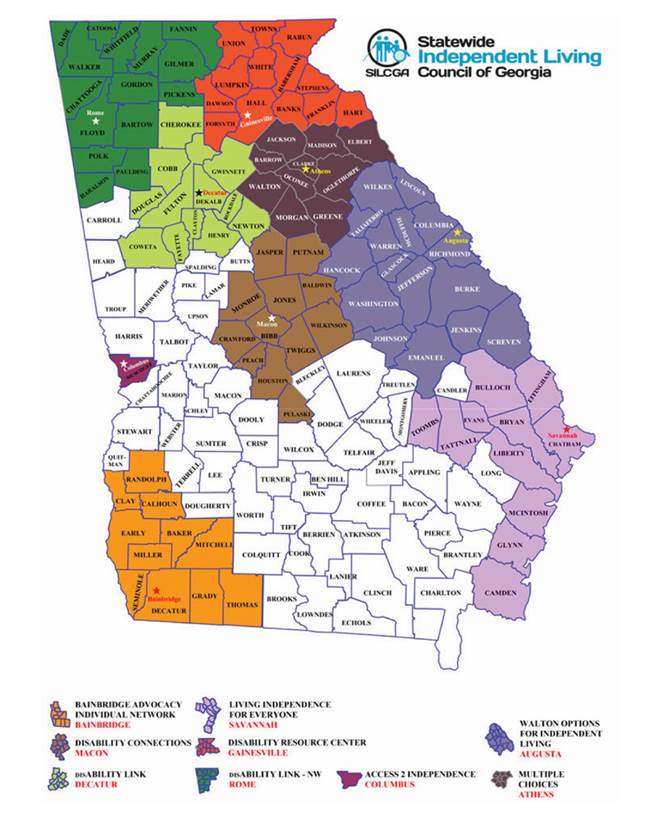
I. GEORGIA ASSOCIATION OF REGIONAL COMMISSIONS (http://garc.ga.gov)
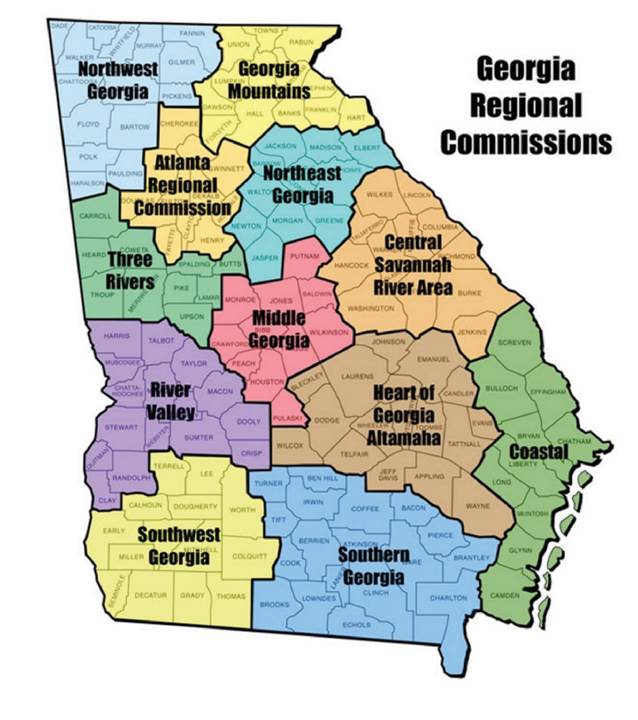
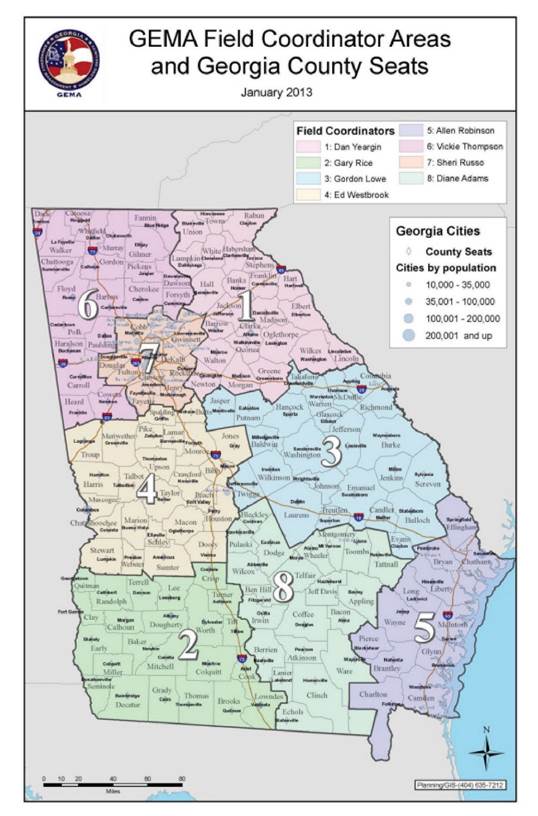
|
Type
|
Authority
|
Description
|
|
Assisted Living
|
Authority
O.C.G.A, Secs. 31-2-7 and 31-7-1
et seq.
|
"Assisted
living community" or "community" means a personal care home
serving 25 residents or more that is licensed by the department to provide
assisted living care.
"Assisted
living care" means the specialized care and services provided by an assisted
living community which includes, the provision of personal services, the
administration of medications by a certified medication aide and the
provision of assisted self- preservation.
Assisted living
services. such as help with grooming, bathing, taking medications and
ambulation, are called "personal services." Communities that
offer personal care services in Georgia are different from nursing homes in
that they do not provide skilled nursing care to patients. Assisted living
is for seniors who require a lesser amount of assistance and medical care
than residents of nursing homes, and who are still able to enjoy an amount
of independence from a caretaker.
|
|
Boarding
Home
|
(For more information, contact the local
Business License and Inspections Department or Planning Commission.)
|
A boarding home
is a congregate living arrangement between landlord and tenant in which the
tenant may share the common areas of the home, a bedroom and bath with other
tenants.
The provision of
laundry services, transportation, money management, and activities are
established by the landlord and tenant.
The landlord
shall not provide supervision of person, supervision of medications,
assistance with activities of daily living, or nursing services.
A list of
available boarding homes in a community will be listed in the ESP database
and accessed for free by calling the Area Agency on Aging at 1-866-552-4464.
|
|
Community Living Arrangement
|
Authority O.C.G.A. Sec. 37-1-22
|
Any residence.
whether operated as a for profit or not for profit, that undertakes through
its ownership or management to provide or arrange for the provision of daily
personal services, supports, care, or treatment exclusively for two or more
adults who are not related to the owner or administrator by blood or marriage
CLAs are
financially supported, in whole or in part by funds designated through the
Department of Behavioral Health and Addictive Diseases.
'Personal
services' means provision of services, on a daily basis, that include, but
are not limited to, individual assistance with or supervision of
medications, ambulation and transfer, and essential activities of daily
living such as eating, bathing, grooming, dressing, and toileting.
'Supports, care,
or treatment' means specific services that are provided to the resident in
the Community Living Arrangement, coordinated by the administrator as
necessary or reasonably requested by the resident and that include but are
not limited to: mental health services, habilitation, rehabilitation. social
services, medical, dental, and other health care services, education,
financial management, legal services, vocational services, transportation,
recreational and leisure activities, and other services required to meet a
resident's needs.
|
|
Personal Care Home
|
Authority O.C.G.A. Secs. 31-7-2.1,
37-7-12
|
"Any
dwelling, whether operated for profit or not, which undertakes through its
ownership or management to provide or arrange for the provision of housing,
food service, and one or more personal services."
For two or more
adults who are not related to the owner or administrator by blood or
marriage;
'Personal
Services' includes, but is not limited to, individual assistance with or
supervision of self-administered medication, assistance with ambulation and
transfer and essential activities of daily living such as eating, bathing,
grooming, dressing, and toileting;"
|
|
Private Home Care
|
Authority O.C.G.A. Sec. 300 et seq.
|
'Private home
care provider or provider' means any person, business entity, corporation.
or association, whether operated for profit or not for profit, that directly
provides or makes provision for private home care services through:
1) its own
employees or agents;
2) contractual
arrangements with independent contractors; or
3) referral of other
persons to render home care services, when the individual making the
referral has ownership or financial interest in the delivery of those services
by those other persons who would deliver those services.
'Private home
care services' means those items and services provided at a patient's
residence that involve direct care to that patient and includes, without
limitation, any or all of the following: 1) nursing services, provided that
such services can only be provided by a person licensed as a Registered
Professional Nurse or licensed Practical Nurse in accordance with applicable
professional licensing statutes and associated rules; 2) personal care tasks;
and 3) companion or sitter tasks.
Private home
care services shall not include physical, speech, or occupational therapy;
medical nutrition therapy; medical social services; or home health aide
services provided by a home health agency.
'Residence'
means the place where an individual makes that person's permanent or
"temporary home, whether that person's own apartment or house, a friend
or relative's home, or a personal care home, but shall not include a
hospital, nursing home, hospice, or other health care facility licensed
under Chapter 31-7-1 et seq.
'Personal care
tasks means assistance with bathing, toileting, grooming, shaving, dental
care, dressing, and eating; and may include but is not limited to proper nutrition,
home management, housekeeping tasks, ambulation and transfer, and medically related
activities, including the taking of vital signs only in conjunction with the
above tasks.
'Companion or
sitter tasks means the following tasks which are provided to elderly,
handicapped, or convalescing individuals: transport and escort services; meal
preparation and serving; and household tasks essential to cleanliness and
safety."
|
(For more information, contact Healthcare
Facilities Regulation at 1-800-878-6442.)